On this page:
- What is a balance disorder?
- What are the symptoms of a balance disorder?
- What causes balance disorders?
- How does my body keep its balance?
- What are some types of balance disorders?
- How are balance disorders diagnosed?
- How are balance disorders treated?
- When should I seek help if I think I have a balance disorder?
- How can I help my doctor make a diagnosis?
- What research is being done on balance disorders?
- Where can I find additional information about balance disorders?
What is a balance disorder?
A balance disorder is a condition that makes you feel unsteady or dizzy. If you are standing, sitting, or lying down, you might feel as if you are moving, spinning, or floating. If you are walking, you might suddenly feel as if you are tipping over.
Everyone has a dizzy spell now and then, but the term “dizziness” can mean different things to different people. For one person, dizziness might mean a fleeting feeling of faintness, while for another it could be an intense sensation of spinning (vertigo) that lasts a long time.
About 15 percent of American adults (33 million) had a balance or dizziness problem in 2008. Balance disorders can be caused by certain health conditions, medications, or a problem in the inner ear or the brain. A balance disorder can profoundly affect daily activities and cause psychological and emotional hardship.
What are the symptoms of a balance disorder?
If you have a balance disorder, your symptoms might include:
- Dizziness or vertigo (a spinning sensation).
- Falling or feeling as if you are going to fall.
- Staggering when you try to walk.
- Lightheadedness, faintness, or a floating sensation.
- Blurred vision.
- Confusion or disorientation.
Other symptoms might include nausea and vomiting; diarrhea; changes in heart rate and blood pressure; and fear, anxiety, or panic. Symptoms may come and go over short time periods or last for a long time, and can lead to fatigue and depression.
What causes balance disorders?
Causes of balance problems include medications, ear infection, a head injury, or anything else that affects the inner ear or brain. Low blood pressure can lead to dizziness when you stand up too quickly. Problems that affect the skeletal or visual systems, such as arthritis or eye muscle imbalance, can also cause balance disorders. Your risk of having balance problems increases as you get older.
Unfortunately, many balance disorders start suddenly and with no obvious cause.
How does my body keep its balance?
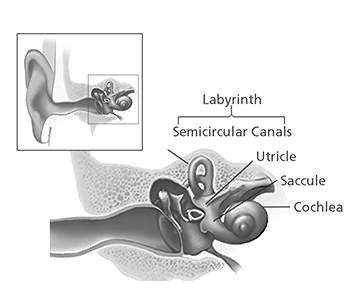
Your sense of balance relies on a series of signals to your brain from several organs and structures in your body, specifically your eyes, ears, and the muscles and touch sensors in your legs. The part of the ear that assists in balance is known as the vestibular system, or the labyrinth, a maze-like structure in your inner ear made of bone and soft tissue.
Structures of the balance system inside the inner ear
Source: NIH/NIDCD
Within the labyrinth are structures known as semicircular canals. The semicircular canals contain three fluid-filled ducts, which form loops arranged roughly at right angles to one another. They tell your brain when your head rotates. Inside each canal is a gelatin-like structure called the cupula [KEW-pyew-lah], stretched like a thick sail that blocks off one end of each canal. The cupula sits on a cluster of sensory hair cells. Each hair cell has tiny, thin extensions called stereocilia that protrude into the cupula.
When you turn your head, fluid inside the semicircular canals moves, causing the cupulae to flex or billow like sails in the wind, which in turn bends the stereocilia. This bending creates a nerve signal that is sent to your brain to tell it which way your head has turned.
Between the semicircular canals and the cochlea (a snail-shaped, fluid-filled structure in the inner ear) lie two otolithic [oh-toe-LITH-ic] organs: fluid-filled pouches called the utricle [YOU-trih-cull] and the saccule [SACK-kewl]. These organs tell your brain the position of your head with respect to gravity, such as whether you are sitting up, leaning back, or lying down, as well as any direction your head might be moving, such as side to side, up or down, forward or backward.
The utricle and the saccule also have sensory hair cells lining the floor or wall of each organ, with stereocilia extending into an overlying gel-like layer. Here, the gel contains tiny, dense grains of calcium carbonate called otoconia [oh-toe-CONE-ee-ah]. Whatever the position of your head, gravity pulls on these grains, which then move the stereocilia to signal your head's position to your brain. Any head movement creates a signal that tells your brain about the change in head position.
When you move, your vestibular system detects mechanical forces, including gravity, that stimulate the semicircular canals and the otolithic organs. These organs work with other sensory systems in your body, such as your vision and your musculoskeletal sensory system, to control the position of your body at rest or in motion. This helps you maintain stable posture and keep your balance when you're walking or running. It also helps you keep a stable visual focus on objects when your body changes position.
When the signals from any of these sensory systems malfunction, you can have problems with your sense of balance, including dizziness or vertigo. If you have additional problems with motor control, such as weakness, slowness, tremor, or rigidity, you can lose your ability to recover properly from imbalance. This raises the risk of falling and injury.
What are some types of balance disorders?
There are more than a dozen different balance disorders. Some of the most common are:
- Benign paroxysmal positional vertigo (BPPV) or positional vertigo: A brief, intense episode of vertigo triggered by a specific change in the position of the head. You might feel as if you're spinning when you bend down to look under something, tilt your head to look up or over your shoulder, or roll over in bed. BPPV occurs when loose otoconia tumble into one of the semicircular canals and affect how the cupula works. This keeps the cupula from flexing properly, sending incorrect information about your head's position to your brain, and causing vertigo. BPPV can result from a head injury, or can develop just from getting older.
- Labyrinthitis: An infection or inflammation of the inner ear that causes dizziness and loss of balance. It is often associated with an upper respiratory infection, such as the flu.
- Ménière's disease: Episodes of vertigo, hearing loss, tinnitus (a ringing or buzzing in the ear), and a feeling of fullness in the ear. It may be associated with a change in fluid volume within parts of the labyrinth, but the cause or causes are still unknown. For more information, read the NIDCD fact sheet Ménière's Disease.
- Vestibular neuronitis: An inflammation of the vestibular nerve that can be caused by a virus, and primarily causes vertigo.
- Perilymph fistula: A leakage of inner ear fluid into the middle ear. It causes unsteadiness that usually increases with activity, along with dizziness and nausea. Perilymph fistula can occur after a head injury, dramatic changes in air pressure (such as when scuba diving), physical exertion, ear surgery, or chronic ear infections. Some people are born with perilymph fistula.
- Mal de Debarquement syndrome (MdDS): A feeling of continuously rocking, swaying, or bobbing, typically after an ocean cruise or other sea travel, or even after prolonged running on a treadmill. Usually the symptoms go away within a few hours or days after you reach land or stop using the treadmill. Severe cases, however, can last months or even years, and the cause remains unknown.
How are balance disorders diagnosed?
Diagnosis of a balance disorder is difficult. To find out if you have a balance problem, your primary doctor may suggest that you see an otolaryngologist and an audiologist. An otolaryngologist is a physician and surgeon who specializes in diseases and disorders of the ear, nose, neck, and throat. An audiologist is a clinician who specializes in the function of the hearing and vestibular systems.

Dislodging otoconia using the Epley maneuver.
Source: NIH/NIDCD
You may be asked to participate in a hearing examination, blood tests, a video nystagmogram (a test that measures eye movements and the muscles that control them), or imaging studies of your head and brain. Another possible test is called posturography. For this test, you stand on a special movable platform in front of a patterned screen.
Posturography measures how well you can maintain steady balance during different platform conditions, such as standing on an unfixed, movable surface. Other tests, such as rotational chair testing, brisk head-shaking testing, or even tests that measure eye or neck muscle responses to brief clicks of sound, may also be performed. The vestibular system is complex, so multiple tests may be needed to best evaluate the cause of your balance problem.
How are balance disorders treated?
The first thing an otolaryngologist will do if you have a balance problem is determine if another health condition or a medication is to blame. If so, your doctor will treat the condition, suggest a different medication, or refer you to a specialist if the condition is outside his or her expertise.
If you have BPPV, your otolaryngologist or audiologist might perform a series of simple movements, such as the Epley maneuver, to help dislodge the otoconia from the semicircular canal. In many cases, one session works; other people need the procedure several times to relieve their dizziness.
If you are diagnosed with Ménière's disease, your otolaryngologist may recommend that you make some changes to your diet and, if you are a smoker, that you stop smoking. Anti-vertigo or anti-nausea medications may relieve your symptoms, but they can also make you drowsy. Other medications, such as gentamicin (an antibiotic) or corticosteroids may be used. Although gentamicin may reduce dizziness better than corticosteroids, it occasionally causes permanent hearing loss. In some severe cases of Ménière's disease, surgery on the vestibular organs may be needed.
Some people with a balance disorder may not be able to fully relieve their dizziness and will need to find ways to cope with it. A vestibular rehabilitation therapist can help you develop an individualized treatment plan.
Talk to your doctor about whether it's safe to drive, and about ways to lower your risk of falling and getting hurt during daily activities, such as when you walk up or down stairs, use the bathroom, or exercise. To reduce your risk of injury from dizziness, avoid walking in the dark. Wear low-heeled shoes or walking shoes outdoors. If necessary, use a cane or walker and modify conditions at your home and workplace, such as adding handrails.
When should I seek help if I think I have a balance disorder?
To help you decide whether to seek medical help for dizziness or balance problems, ask yourself the following questions. If you answer “yes” to any of these questions, talk to your doctor:
- Do I feel unsteady?
- Do I feel as if the room is spinning around me, even for a very brief time?
- Do I feel as if I'm moving when I know I'm sitting or standing still?
- Do I lose my balance and fall?
- Do I feel as if I'm falling?
- Do I feel lightheaded or as if I might faint?
- Do I have blurred vision?
- Do I ever feel disoriented—losing my sense of time or location?
How can I help my doctor make a diagnosis?
You can help your doctor make a diagnosis and determine a treatment plan by answering the questions below. Be prepared to discuss this information during your appointment.
- The best way I can describe my dizziness or balance problem is:
- Is there a spinning sensation, and if so, which way does the room spin?
- Is the dizziness/spinning caused by any specific motion or does it occur even when sitting or lying still?
- Are there any other symptoms that occur at the same time as the dizziness/spinning, such as hearing loss, tinnitus, a feeling of pressure in one or both ears, or a headache?
- Does anything seem to help the dizziness/spinning?
- How often do I feel dizzy or have trouble keeping my balance? How long do the dizziness or spinning episodes last (seconds, minutes, hours, days)?
- Have I ever fallen?
- When did I fall?
- Where did I fall?
- Under what conditions did I fall?
- How often have I fallen?
- These are the medicines I take. Include all prescription medications; all over-the-counter medicine, such as aspirin, antihistamines, or sleep aids; and all vitamin supplements and alternative or homeopathic remedies:
- Name of medicine or supplement: ______________________.
- How much (milligrams) _____ and how often (times) ______ per day.
- The condition I take this medicine for is: __________________________.
What research is being done on balance disorders?
Scientists supported by the National Institute on Deafness and Other Communication Disorders (NIDCD) are studying animal ears to learn if inner-ear structures that help with balance but are destroyed by aging, medications, infections, or trauma can someday be regrown in people with balance problems. Other NIDCD-supported scientists are testing vestibular prostheses—miniature devices that may be worn outside the body or implanted into the ear to regulate the function of balance organs in the inner ear and ease dizziness. Some of these devices are being tested on volunteers in clinical trials, and others are still being developed. Visit the NIH Clinical Research Trials and You website to read about these and other clinical trials that are recruiting volunteers.
NIDCD-funded scientists are also working to develop much-needed tests to appropriately diagnose balance disorders. Standardized tests will help doctors determine the best way to help individuals restore their sense of balance and quality of life. These tests will also help us understand how many people suffer from balance disorders, and track whether the sense of balance is restored following treatment.
Where can I find additional information about balance disorders?
The NIDCD maintains a directory of organizations that provide information on the normal and disordered processes of hearing, balance, taste, smell, voice, speech, and language.
For more information, contact us at:
NIDCD Information Clearinghouse
1 Communication Avenue
Bethesda, MD 20892-3456
Toll-free voice: (800) 241-1044
Toll-free TTY: (800) 241-1055
Email: nidcdinfo@nidcd.nih.gov
NIH Pub. No. 00-4374
December 2017