Note: Budget requests for years prior to FY 2026 were submitted by prior Administrations and may not reflect current HHS policy.
- Download Congressional Justification 2025 (2.1MB PDF)
FY 2025 Budget
DEPARTMENT OF HEALTH AND HUMAN SERVICES
NATIONAL INSTITUTES OF HEALTH
National Institute on Deafness and Other Communication Disorders (NIDCD)
On this page:
- Director’s Overview
- NIDCD Fact Sheet
- Major Changes in the Budget Request
- Budget Mechanism Table
- Appropriations Language
- Summary of Changes
- Budget Graphs
- Organization Chart
- Budget Authority by Activity Table
- Justification of Budget Request
- Appropriations History
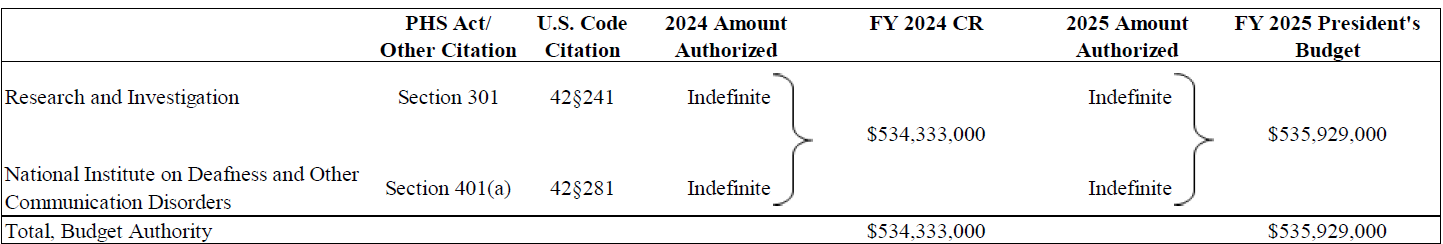
- Authorizing Legislation
- Amounts Available for Obligation
- Budget Authority by Object Class
- Salaries and Expenses
- Detail of Full-Time Equivalent Employment (FTE)
- Detail of Positions
General Notes
- FY 2024 funding levels cited in this document are based on the Continuing Resolution in effect at the time of budget preparation (Public Law 118-35) and do not include HIV/AIDS transfers.
- Detail in this document may not sum to the subtotals and totals due to rounding.
Director’s Overview

M.D., M.S., M.B.A.
Director, NIDCD
About one in six Americans have a hearing, balance, sensory, or other communication disorder. For these individuals, the basic components of communication — sensing, interpreting, and responding to people and things in our environment — can be challenging. The National Institute on Deafness and Other Communication Disorders (NIDCD) manages a broad portfolio of basic, translational, clinical, and public health research focused on human communication and associated disorders in three program areas: hearing and balance; taste and smell; and voice, speech, and language. NIDCD’s vision is to advance the science of communication to improve lives.
Making NIDCD discoveries accessible and affordable: NIDCD has long supported research to provide the evidence-base for new service delivery models to improve accessibility and affordability of hearing health care. In October 2022, a notable achievement of this research was the FDA establishing a new category of over the counter (OTC) hearing aids for Americans with perceived mild to moderate hearing loss. The new rule allows consumers to buy directly in stores and online, without visiting a hearing health professional for an examination. By making hearing aids less expensive and easier to obtain, these new regulations may increase the uptake and sustained use of hearing aids by almost 30 million adults in the United States who could benefit from hearing aid use. Improving accessible and affordable hearing health care is especially important given the association with hearing loss and cognitive decline. Recent evidence from an NIH-funded clinical trial suggests that treating hearing loss can slow down loss of thinking and memory abilities by 48 percent over 3 years in older adults at increased risk for cognitive decline.1 In an extension of this trial, NIDCD is supporting a study that tests whether telehealth services improve long-term hearing aid use as compared to conventional, in office, hearing health care delivery in a large population of racially-diverse, older adults who already use hearing aids. The study will also compare telehealth versus conventional hearing health care services on outcomes of social, mental, physical, and cognitive functioning after one year in the trial.2 This is just one example of a number of NIDCD-funded hearing health care studies that support innovative clinical and translational research strategies to improve access to and affordability of hearing health care for adults.
NIDCD has also advanced health care that is more accessible and affordable in the NIDCD smell (olfaction) mission area. Olfactory disorders negatively impact quality of life. Loss of smell affects up to 30-80 percent of people who get COVID-19, depending on the variant of SARS-CoV-2 viral infection.3 Tests have been developed that measure total (anosmia) or partial (hyposmia) loss of smell. However, these tests are difficult and costly to carry out on a widespread scale during a pandemic. To make screening for olfactory disorders more affordable and accessible, NIDCD has supported investigators to develop rapid, inexpensive, and self-administered smell tests that can detect and discriminate between different types of olfactory disorders.4,5 These new tests provide an option for population-wide surveillance of smell function in a wide range of settings, including during a pandemic. Similarly, these smell tests may also be used to detect early signs of other serious health conditions like Parkinson’s disease, where hyposmia is a frequent symptom, so that patients can receive early treatment. These examples highlight how NIDCD supports applied research, experimental development, pre-commercialization, and standards-related efforts that will facilitate the adoption of a broad range of new technologies.
Launching a new initiative for speech and language developmental delays: Speech delay, or ‘late talking’ is diagnosed when a child, usually over the age of 18 months, is not meeting expressive language milestones. Long-term outcomes for late talking children vary, and the unique early indicators and developmental consequences are not fully understood. In early 2023, NIH launched the Tackling Acquisition of Language in Kids (TALK) initiative that will build a more robust knowledge base to support late talking children. It has since grown into an initiative with engagement across five NIH institutes. NIDCD and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) co-lead the initiative with participation from the National Institute of Neurological Disorders and Stroke (NINDS), the National Institute of Mental Health (NIMH), and the National Center for Advancing Translational Sciences (NCATS).

The purpose of the TALK initiative is to advance understanding of why children with various conditions or risk factors are late to talk; define developmental trajectories that lead to better outcomes; and evaluate the effectiveness of clinical approaches to improve language outcomes. Through this initiative, NIH aims to fill knowledge gaps and work toward the overarching goals of this initiative, including gathering, storing, and evaluating data to understand longitudinal development in late talking children, and providing caregivers and clinicians with state-of-the-science information on supporting late talkers. To achieve this, NIH funded several research grants, provided supplemental funding in 2023 to relevant ongoing awards, and published two Notices of Funding Opportunities to solicit applications.6,7 A long-term goal of the initiative is to provide parents, caregivers, educators, and health care professionals the information they need to help late talking children grow and thrive in school and life.
Setting NIDCD research priorities: NIDCD developed the 2023-2027 Strategic Plan after an iterative and public process through which industry, patient and consumer groups, professional organizations, government partners, and the scientific community were engaged.8 The plan details ambitious and achievable themes and goals that will further the scientific understanding of basic biological systems, disordered human mechanisms, and promising treatments for people with hearing loss or communication disorders. New scientific priorities include precision medicine, translational research, and dissemination and implementation of evidence-based medicine to accelerate innovative, patient-centered treatments into standard clinical care. New to this plan, NIDCD challenges researchers and clinicians to harness biomedical databases, artificial intelligence, and machine learning to improve the lives of those with deafness and communication disorders.
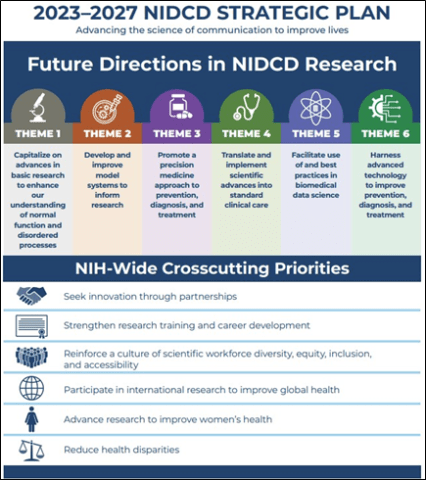
The new plan also includes a strategic focus on diversity, equity, inclusion, and accessibility (DEIA) efforts to diversify the scientific workforce. The Institute recognizes the critical need to address barriers that interfere with the scientific aspirations of individuals from diverse backgrounds, including women and minorities, individuals with disabilities, and individuals from rural areas and other underserved populations. NIDCD is working to increase the number of individuals from diverse backgrounds in the research pipeline in NIDCD scientific mission areas. NIDCD supports fellowship, career development, and mentorship opportunities at universities and institutions nationwide (extramural training) as well as at NIDCD laboratories and clinics in Bethesda, Maryland (intramural training).9 International research training opportunities are also available. NIDCD recognizes that our ability to remain global leaders in scientific discovery and innovation depends upon a pool of highly talented scientists from diverse backgrounds and in broadened public participating and community engagement in R&D.
Facilitating best practices in biomedical data science for hearing health care: NIDCD seeks to maximize the value of data generated through NIDCD-funded research by prioritizing efforts to share biomedical and behavioral data in ways that encourage ongoing use by the entire scientific community. To achieve this goal, NIDCD encourages researchers to preserve and share scientific data using a repository to improve the FAIRness (Findable, Accessible, Interoperable, and Re-usable) of the data. The data in repositories should be standardized and structured in such a way that they are shareable and usable with other repositories. However, to date, the field of adult hearing health care lacks outcome measures that are quantifiable, objective, and correlate in clinically meaningful ways to the person’s lived experience. To address this critical gap, NIDCD is sponsoring an expert committee with the National Academies of Sciences, Engineering, and Medicine called Meaningful Outcome Measures in Adult Hearing Health Care.10 The committee will determine 1) a core set of existing standard outcome measures and 2) recommendations to guide the development of new measures that are appropriate for use in different listening environments. This partnership with the National Institute on Aging, Department of Defense, Centers for Disease Control and Prevention, and Department of Veteran Affairs is an important first step to establish common data elements, one type of health data standard that can help researchers normalize data across studies. This provides the ability to connect and share data seamlessly between computerized systems and allows for the information exchange between other applications and databases. Shared and meaningful scientific data gives researchers the opportunity to accelerate biomedical research discovery, enable validation of results by independent groups, improve accessibility to large datasets that allows for high impact questions through secondary analyses, and promote data reuse across research studies. This effort will also provide industry with widely endorsed meaningful measures to assess benefit of newly developed therapeutics.
Saving lives through advances in science and health: NIDCD has been able to expand support for innovative clinical trials that may one day lead to prevention strategies and treatments that improve the quality of life for individuals who have communication disorders. For example, NIDCD supports clinical trials to help people with severe speech and physical impairment regain their ability to communicate. Conditions such as brainstem stroke or amyotrophic lateral sclerosis (ALS) can rob an individual of their ability to speak, although they retain the ability to think clearly and the desire to communicate with others. Over 25 years ago, these individuals were “locked-in” with no hope of communicating with the outside world.11 Over the last two decades, brain-computer interface (BCI) technology has made some communication possible. BCI technology uses electrodes to analyze brain electrical activity as an individual thinks about speaking or writing, and decodes words and sentences based on the activity. In a recent advance, one research team developed a BCI algorithm that enabled a paralyzed woman to speak through a digital avatar.12 The algorithm improved the speed of synthesized speech, which was personalized to match her voice from before her injury, and it could decode facial movements to animate the avatar. Another research team recently developed an algorithm that could decode speech 3.4 times faster than the previous record and started to approach the speed of natural conversation.13 While there were some errors (incorrect words or word placement in sentences), these proof-of-concept trials are significant advances to restoring more natural communication to people who have lost their ability to speak.
NIDCD Fact Sheet
Advancing the science of communication to improve lives

M.D., M.S., M.B.A.
Director, NIDCD
For over 30 years, NIDCD’s focus has been to bring national attention to normal and disordered processes of hearing, balance, taste, smell, voice, speech, and language and to contribute to advances in biomedical and behavioral research that will improve the lives of the tens of millions of Americans with deafness and other communication disorders. NIDCD employs a wide range of research approaches such as molecular genetics, biomedical imaging, cellular biology, nanotechnology, psychoacoustics, and structural and functional biology to advance the development of better diagnostics, prevention strategies, and treatments.
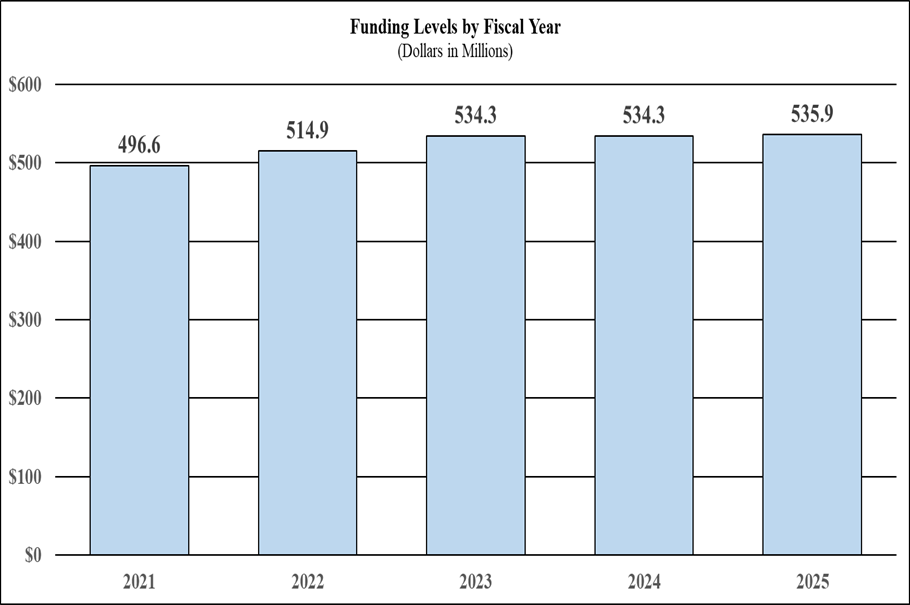
Funding History
President’s Budget 2025: $535,929,000
FY 2024: $534,333,000
FY 2023: $534,330,000
FY 2022: $514,882,000
FY 2021: $496,578,000
FY 2020: $490,692,000
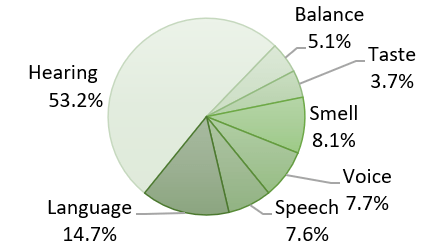
Funding by Mission Area (FY 2023)
Device Detects Loss of Smell After COVID-19

Loss of smell affects up to 80 percent of people who get COVID-19, depending on the variant of SARS-CoV-2 viral infection. Tests have been developed that measure total (anosmia) or partial (hyposmia) loss of smell. However, these tests are difficult and costly to carry out on a widespread scale during a pandemic. To make screening for olfactory disorders more affordable and accessible, NIDCD has supported investigators to develop rapid, inexpensive, and self-administered smell tests that can detect and discriminate between different types of olfactory disorders. Similarly, these smell tests may also be used to detect early signs of other serious health conditions like Parkinson’s disease, where hyposmia is a frequent symptom, so that patients can receive early treatment.
FY 2023 Facts and Figures
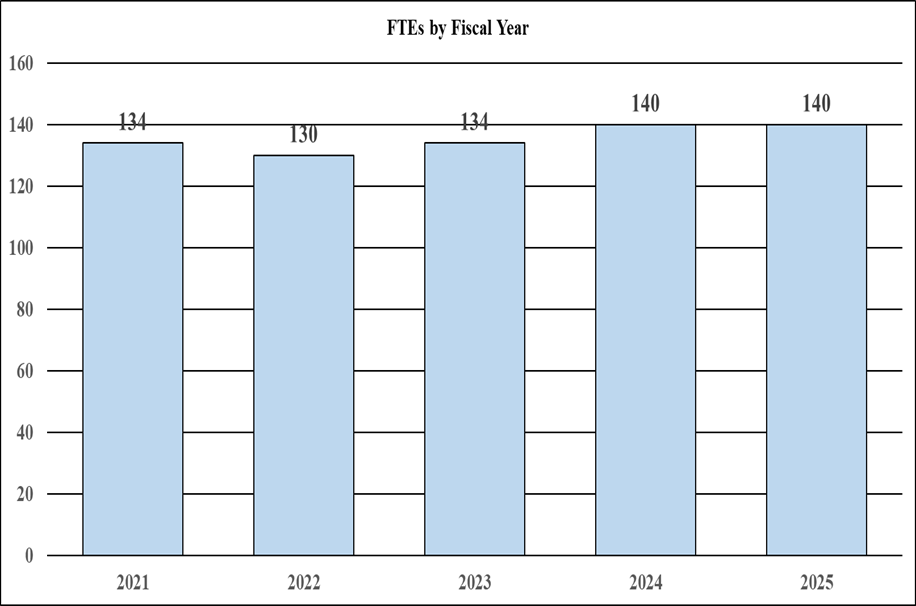
- 134 Full Time Equivalent Employees
- 212 Principal Investigators
- 27.1% Success Rate (R01)
- 23.8% Early-Stage Investigator Success Rate (R01)
- 183 Competing Research Project Grants
- 51 Competing Individual and Institutional Training Awards
Brain Computer Interface Technology
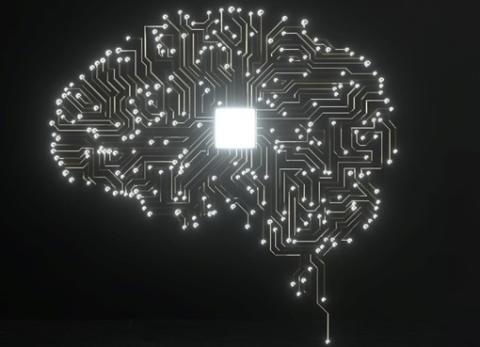
Conditions such as stroke and neurodegenerative disease can cause people to lose the ability to speak. Researchers have been working to develop brain-computer interfaces (BCI) technology that help these people regain their ability to communicate. BCI technology uses electrodes to analyze brain electrical activity as an individual thinks about speaking or writing, and decodes words and sentences based on the activity. NIDCD-funded researchers have developed BCI algorithms that enabled a paralyzed woman to speak through a digital avatar and decode speech approaching the speed of natural conversation. This proof-of-concept trial is a significant advance to restoring more natural communication to people who have lost their ability to speak due to injury or disease.
Tackling Acquisition of Language in Kids (TALK) Initiative

In early 2023, the National Institutes of Health (NIH) launched the Tackling Acquisition of Language in Kids (TALK) Initiative. It has since grown into an initiative with engagement across five institutes co-led by NIDCD and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD). The purpose of the TALK Initiative is to advance understanding of why children with various conditions or risk factors are late to talk; define developmental trajectories that lead to better outcomes; and evaluate the effectiveness of clinical approaches to improve language outcomes. The goal is to provide parents, caregivers, educators, and health care professionals with the information they need to help late talking children grow and thrive in school and life.
Strategic Focus on Data Science

The 2023-2027 NIDCD Strategic Plan was developed using an iterative and public process engaging scientists and community partners. New to this plan, NIDCD challenges researchers to harness biomedical databases, artificial intelligence, and machine learning to improve the lives of those with deafness and communication disorders. The goal is to maximize the value of data generated through NIH-funded research by prioritizing efforts to share biomedical and behavioral data. Shared and meaningful scientific data gives researchers the opportunity to accelerate biomedical research discovery, enable validation of results by independent groups, improve accessibility to large datasets, and promote data reuse across research studies. This effort will also provide meaningful measures to assess benefit of newly developed therapeutics.
Major Changes in the Budget Request
Major changes by budget mechanism and/or budget activity detail are briefly described below. Note that there may be overlap between budget mechanism and activity detail and these highlights will not sum to the total change for the FY 2025 President’s Budget for the National Institute on Deafness and Other Communication Disorders (NIDCD), which is $1.6 million above the FY 2023 Final level, for a total of $535.9 million. Within this funding level, NIDCD will support a diversity mentoring program and a new contract to enhance clinical trials oversight and analysis.
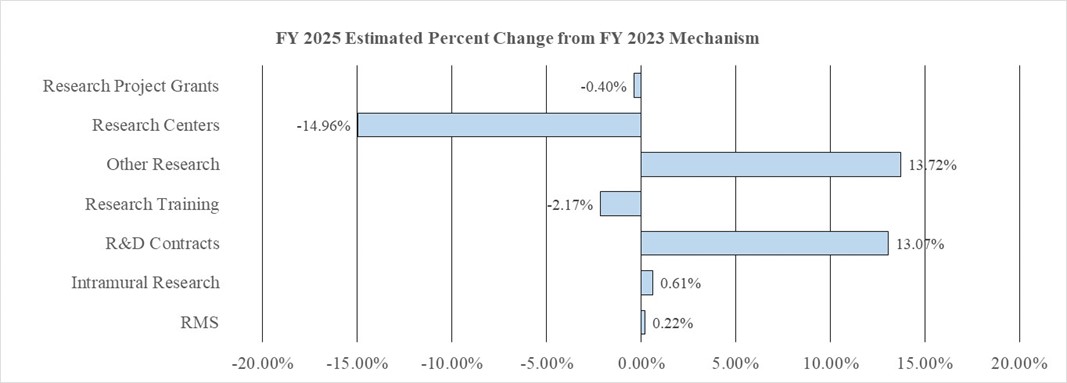
Competing Research Projects (-$3.3 million; total $84.5 million):
NIDCD will fund 177 Competing Research Project awards in FY 2025, a decrease of 6 from the FY 2023 Final level.
Research Centers (-$2.8 million; total $15.7 million):
NIDCD will fund 6 Research Center awards in FY 2025, a decrease of 1 from the FY 2023 Final level.
Other Research (+$2.8 million; total $22.9 million):
NIDCD will fund 123 Other Research awards in FY 2025, an increase of 12 from the FY 2023 Final level. This increase will support NIDCD’s mentored research pathway for otolaryngology residents and medical students program which targets under-represented communities.
Research & Development (R&D) Contracts (+$3.0 million; total $26.3 million):
NIDCD will fund 45 R&D Contracts in FY 2025, an increase of 1 from the FY 2023 Final level. This increase will be used to fund a new clinical trials support contract.
| (Dollars in Thousands) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Mechanism | FY 2023 Final | FY 2024 CR | FY 2025 President's Budget | FY 2025 +/- FY 2023 | ||||
| Number | Amount | Number | Amount | Number | Amount | Number | Amount | |
| Research Projects: | ||||||||
| Noncompeting | 576 | $263,385 | 577 | $267,943 | 577 | $267,950 | 1 | $4,565 |
| Administrative Supplements | (65) | $6,081 | (46) | $3,500 | (41) | $3,250 | -(24) | -$2,831 |
| Competing: | ||||||||
| Renewal | 39 | $20,893 | 39 | $21,120 | 39 | $21,120 | 0 | $227 |
| New | 144 | $66,845 | 138 | $63,350 | 138 | $63,350 | -6 | -$3,495 |
| Supplements | 0 | $0 | 0 | $0 | 0 | $0 | 0 | $0 |
| Subtotal, Competing | 183 | $87,738 | 177 | $84,470 | 177 | $84,470 | -6 | -$3,268 |
| Subtotal, RPGs | 759 | $357,204 | 754 | $355,913 | 754 | $355,670 | -5 | -$1,534 |
| SBIR/STTR | 19 | $16,401 | 19 | $16,400 | 19 | $16,450 | 0 | $49 |
| Research Project Grants | 778 | $373,605 | 773 | $372,313 | 773 | $372,120 | -5 | -$1,485 |
| Research Centers: | ||||||||
| Specialized/Comprehensive | 7 | $18,515 | 6 | $15,717 | 6 | $15,717 | -1 | -$2,798 |
| Clinical Research | 0 | $0 | 0 | $28 | 0 | $28 | 0 | $28 |
| Biotechnology | 0 | $0 | 0 | $0 | 0 | $0 | 0 | $0 |
| Comparative Medicine | 0 | $0 | 0 | $0 | 0 | $0 | 0 | $0 |
| Research Centers in Minority Institutions | 0 | $0 | 0 | $0 | 0 | $0 | 0 | $0 |
| Research Centers | 7 | $18,515 | 6 | $15,745 | 6 | $15,745 | -1 | -$2,770 |
| Other Research: | ||||||||
| Research Careers | 67 | $10,891 | 68 | $11,064 | 68 | $11,090 | 1 | $199 |
| Cancer Education | 0 | $0 | 0 | $0 | 0 | $0 | 0 | $0 |
| Cooperative Clinical Research | 0 | $0 | 0 | $0 | 0 | $0 | 0 | $0 |
| Biomedical Research Support | 0 | $0 | 0 | $0 | 0 | $0 | 0 | $0 |
| Minority Biomedical Research Support | 0 | $0 | 0 | $0 | 0 | $0 | 0 | $0 |
| Other | 44 | $9,251 | 49 | $10,385 | 55 | $11,815 | 11 | $2,564 |
| Other Research | 111 | $20,142 | 117 | $21,449 | 123 | $22,905 | 12 | $2,763 |
| Total Research Grants | 896 | $412,262 | 896 | $409,507 | 902 | $410,770 | 6 | -$1,492 |
| Ruth L Kirschstein Training Awards: | FTTPs | FTTPs | FTTPs | FTTPs | ||||
| Individual Awards | 136 | $6,655 | 136 | $6,990 | 136 | $7,014 | 0 | $359 |
| Institutional Awards | 143 | $9,096 | 143 | $8,386 | 143 | $8,395 | 0 | -$701 |
| Total Research Training | 279 | $15,751 | 279 | $15,376 | 279 | $15,409 | 0 | -$342 |
| Research & Develop. Contracts | 44 | $23,217 | 45 | $26,250 | 45 | $26,250 | 1 | $3,033 |
| (SBIR/STTR) (non-add) | (0) | ($216) | (0) | ($0) | (0) | ($220) | (0) | ($4) |
| Intramural Research | 58 | $56,359 | 64 | $56,500 | 64 | $56,700 | 6 | $341 |
| Res. Management & Support | 76 | $26,742 | 76 | $26,700 | 76 | $26,800 | 0 | $58 |
| SBIR Admin. (non-add) | ($0) | ($0) | ($0) | ($0) | ||||
| Construction | $0 | $0 | $0 | $0 | ||||
| Buildings and Facilities | $0 | $0 | $0 | $0 | ||||
| Total, NIDCD | 134 | $534,330 | 140 | $534,333 | 140 | $535,929 | 6 | $1,599 |
| *All items in italics and brackets are non-add entries. | ||||||||
Appropriations Language
NATIONAL INSTITUTES OF HEALTH
NATIONAL INSTITUTE ON DEAFNESS AND OTHER COMMUNICATION DISORDERS
For carrying out section 301 and title IV of the PHS Act with respect to deafness and other communication disorders, $535,929,000.
| (Dollars in Thousands) | |||||||
|---|---|---|---|---|---|---|---|
| CHANGES | FY 2023 Final | FY 2025 President's Budget | Built-In Change from FY 2023 Final | ||||
| FTEs | Budget Authority | FTEs | Budget Authority | FTEs | Budget Authority | ||
| 1. Intramural Research: | |||||||
| A. Built-in cost changes: | |||||||
| a. FY 2024 effect of FY 2023 pay & benefits increase | $14,461 | $15,704 | $171 | ||||
| b. FY 2024 effect of FY 2024 pay & benefits increase | $14,461 | $15,704 | $563 | ||||
| c. FY 2024 paid days adjustment | $14,461 | $15,704 | $56 | ||||
| d. Differences attributable to FY 2024 change in FTE | $14,461 | $15,704 | $0 | ||||
| e. FY 2025 effect of FY 2024 pay & benefits increase | $14,461 | $15,704 | $191 | ||||
| f. FY 2025 effect of FY 2025 pay & benefits increase | $14,461 | $15,704 | $260 | ||||
| g. FY 2025 paid days adjustment | $14,461 | $15,704 | $0 | ||||
| h. Differences attributable to FY 2025 change in FTE | $14,461 | $15,704 | $0 | ||||
| i. Payment for centrally furnished services | $8,407 | $9,014 | $607 | ||||
| j. Cost of laboratory supplies, materials, other expenses, and non-recurring costs | $33,491 | $31,982 | $2,411 | ||||
| Subtotal, IR built-in cost changes | $4,259 | ||||||
| 2. Research Management and Support: | |||||||
| A. Built-in cost changes: | |||||||
| a. FY 2024 effect of FY 2023 pay & benefits increase | $16,246 | $17,640 | $192 | ||||
| b. FY 2024 effect of FY 2024 pay & benefits increase | $16,246 | $17,640 | $632 | ||||
| c. FY 2024 paid days adjustment | $16,246 | $17,640 | $63 | ||||
| d. Differences attributable to FY 2024 change in FTE | $16,246 | $17,640 | $0 | ||||
| e. FY 2025 effect of FY 2024 pay & benefits increase | $16,246 | $17,640 | $214 | ||||
| f. FY 2025 effect of FY 2025 pay & benefits increase | $16,246 | $17,640 | $290 | ||||
| g. FY 2025 paid days adjustment | $16,246 | $17,640 | $0 | ||||
| h. Differences attributable to FY 2025 change in FTE | $16,246 | $17,640 | $0 | ||||
| i. Payment for centrally furnished services | $1,852 | $1,986 | $134 | ||||
| j. Cost of laboratory supplies, materials, other expenses, and non-recurring costs | $8,641 | $7,174 | $624 | ||||
| Subtotal, RMS built-in cost changes | $2,148 | ||||||
| CHANGES | FY 2023 Final | FY 2025 President's Budget | Program Change from FY 2023 Final | ||||
|---|---|---|---|---|---|---|---|
| No. | Amount | No. | Amount | No. | Amount | ||
| B. Program: | |||||||
| 1. Research Project Grants: | |||||||
| a. Noncompeting | 576 | $269,466 | 577 | $271,200 | 1 | $1,734 | |
| b. Competing | 183 | $87,738 | 177 | $84,470 | -6 | -$3,268 | |
| c. SBIR/STTR | 19 | $16,401 | 19 | $16,450 | 0 | $49 | |
| Subtotal, RPGs | 778 | $373,605 | 773 | $372,120 | -5 | -$1,485 | |
| 2. Research Centers | 7 | $18,515 | 6 | $15,745 | -1 | -$2,770 | |
| 3. Other Research | 111 | $20,142 | 123 | $22,905 | 12 | $2,763 | |
| 4. Research Training | 279 | $15,751 | 279 | $15,409 | 0 | -$342 | |
| 5. Research and development contracts | 44 | $23,217 | 45 | $26,250 | 1 | $3,033 | |
| Subtotal, Extramural | $451,229 | $452,429 | $1,200 | ||||
| 6. Intramural Research | 58 | $56,359 | 64 | $56,700 | 6 | -$3,917 | |
| 7. Research Management and Support | 76 | $26,742 | 76 | $26,800 | 0 | -$2,091 | |
| 8. Construction | $0 | $0 | $0 | ||||
| 9. Buildings and Facilities | $0 | $0 | $0 | ||||
| Subtotal, program changes | -$4,808 | ||||||
| Total built-in and program changes | 134 | $534,330 | 140 | $535,929 | 6 | $1,599 | |
Budget Graphs
Fiscal Year 2025 Budget Graphs
History of Budget Authority and FTEs:
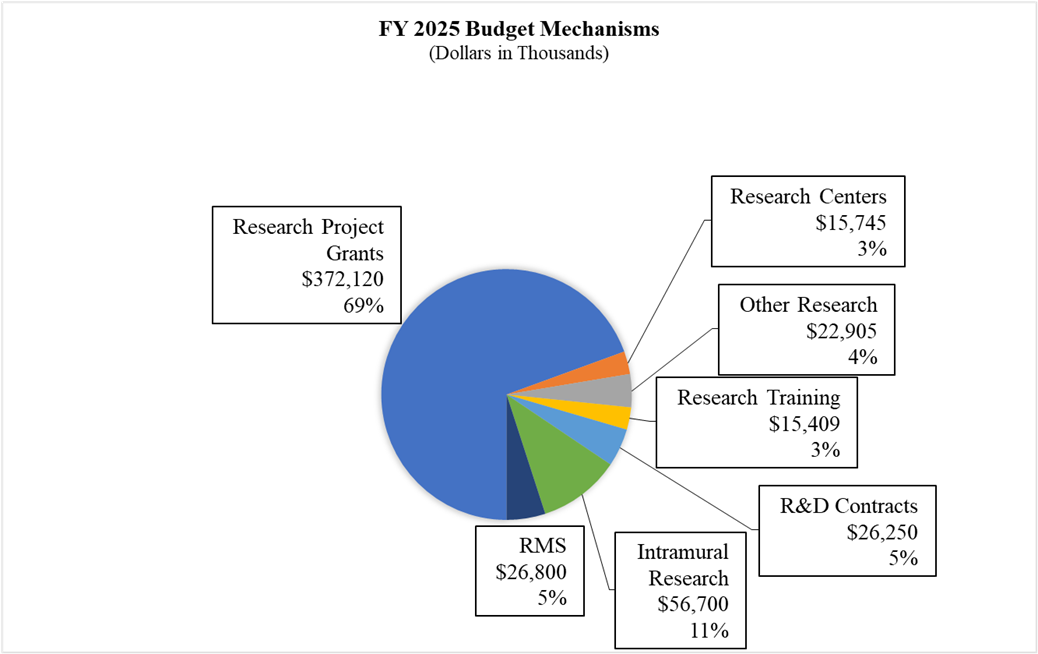
Distribution by Mechanism:
Change by Selected Mechanisms:
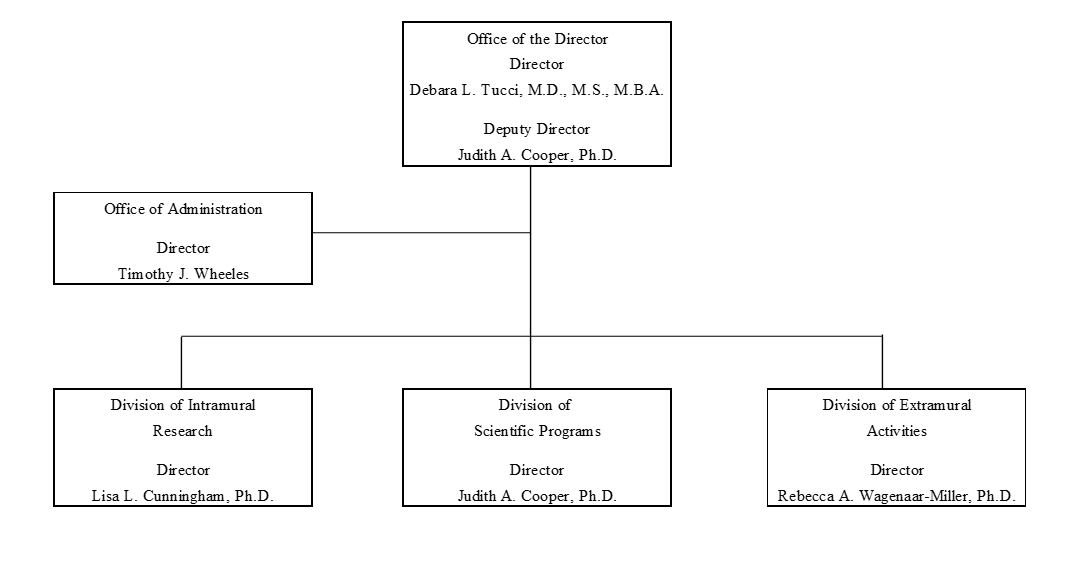
Organization Chart
| (Dollars in Thousands) | ||||||||
|---|---|---|---|---|---|---|---|---|
| FY 2023 Final | FY 2024 CR | FY 2025 President's Budget | FY 2025 +/- FY 2023 Final | |||||
| Extramural Research | FTE | Amount | FTE | Amount | FTE | Amount | FTE | Amount |
| Detail | ||||||||
| Hearing and Balance | $242,696 | $242,644 | $243,341 | $645 | ||||
| Taste and Smell | $57,874 | $57,861 | $58,028 | $154 | ||||
| Voice, Speech, and Language | $150,660 | $150,628 | $151,060 | $401 | ||||
| Subtotal, Extramural | $451,229 | $451,133 | $452,429 | $1,200 | ||||
| Intramural Research | 58 | $56,359 | 64 | $56,500 | 64 | $56,700 | 6 | $341 |
| Research Management & Support | 76 | $26,742 | 76 | $26,700 | 76 | $26,800 | 0 | $58 |
| TOTAL | 134 | $534,330 | 140 | $534,333 | 140 | $535,929 | 6 | $1,599 |
| *Includes FTEs whose payroll obligations are supported by the NIH Common Fund. | ||||||||
| FY 2023 Final | FY 2024 CR | FY 2025 President's Budget | FY 2025 +/- FY 2023 | |
|---|---|---|---|---|
| BA | $534,330,000 | $534,333,000 | $535,929,000 | +$1,599,000 |
| FTE | 134 | 140 | 140 | +6 |
Program funds are allocated as follows: Competitive Grants/Cooperative Agreements; Contracts; Direct Federal/Intramural and Other.
Overall Budget Policy: The FY 2025 President’s Budget request for the National Institute on Deafness and Other Communication Disorders (NIDCD) is $535.9 million, which is $1.6 million over the FY 2023 Final level. This funding level will support basic, translational, and clinical research across all of NIDCD’s mission areas, as described below.
Program Descriptions
Hearing and Balance Program
Loss of hearing or balance imposes a significant social and economic burden upon individuals, their families, and the communities in which they live. Hearing and balance disorders cross all ethnic and socioeconomic lines. The prevalence of hearing loss increases with age, with nearly 25 percent of adults aged 65–74 years old having a disabling hearing loss and up to 50 percent for those who are 75 years old and older.14 Nearly three out of every 1,000 children in the United States are born with a detectable level of hearing loss in one or both ears that can affect their speech, language, social, and cognitive development.15 Further, according to the Centers for Disease Control and Prevention (CDC), falls are the leading cause of injury for adults 65 years and older.16 Accordingly, NIDCD supports research that will lead to improved treatments for, and prevention of, hearing and balance disorders. Research projects in hearing and balance encompass a little over half of NIDCD’s grant portfolio.
Individuals with Usher syndrome (USH) have variable loss of hearing, balance, and vision because the sensory cells in the inner ear and eye develop and function abnormally. Gene therapy is a potential treatment as it can modify a person’s genes to allow for normal sensory cell function. NIDCD funded scientists are examining ways to use gene therapy to restore hearing and balance in individuals with USH. Researchers use viruses to insert corrected copies of genes into target cells. However, some USH genes are too large for this approach. In a recent study, scientists successfully designed and introduced a “mini-gene” for one type of USH.17 This novel approach successfully rescued hearing in mice. The researchers believe this same approach could be used to restore balance and vision. They will next test this gene therapy in other animal models. The findings support growing evidence that gene therapy could be an effective treatment for inherited types of hearing loss and balance disorders.
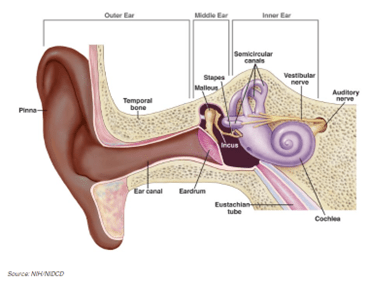
Ear infections, or otitis media (OM), are the most common childhood bacterial infection, and the number one reason children visit the doctor in their first year of life. Overuse of antibiotics in the treatment of OM can contribute to antibiotic resistance, a significant global health issue. Repeated episodes of OM can contribute to hearing loss and possibly delayed language ability. Further, OM represents a substantial societal burden, incurring over $5 billion in direct health care costs and indirect out-of-pocket costs, such as lost wages.18 To address this critical public health concern, NIDCD funds research to accelerate the development of innovative and effective ways to prevent and treat OM. One NIDCD-research study seeks to elucidate the molecular mechanisms of the innate (inborn) immune response to OM infection.19 This information can help identify new therapeutic targets and novel ways to control mucus overproduction, which underlies hearing loss from some types of ear infections. Another NIDCD-funded study is developing ways to deliver drugs across the intact ear drum.20 Local drug delivery would be a highly effective approach to treat OM, and it would also serve to avoid unnecessary side effects of systemic antibiotic treatment and decrease the development of antibiotic resistance.
Individuals who visit the emergency room with symptoms of vertigo or dizziness may be misdiagnosed, resulting in unnecessary, expensive tests and incorrect treatments. Benign paroxysmal positional vertigo (BPPV), or positional vertigo, is a common balance disorder that results in sudden onset of dizziness, spinning or vertigo when moving the head. BPPV can be corrected through a series of simple movements, such as the Epley maneuver, to help dislodge the otoconia (tiny rock-like crystals) that have become lodged in an incorrect location in the inner ear, causing vertigo with certain movements. NIDCD is supporting a clinical trial that tests a strategy to guide clinicians toward evidence-based practices to diagnose and treat dizziness, including BPPV in a real-world setting such as emergency rooms.21 This type of translational research bridges the gap between scientific advances and real-world uptake to improve public health and potentially reduce health care costs.
Exploratory Research Using Invasive Neural Recording and Stimulating Technologies in the Human Brain
NIDCD is leading a funding opportunity through the Brain Research Through Advancing Innovative Neurotechnologies® (BRAIN) Initiative for applications on innovative, high-impact questions in human neuroscience that can be examined during brain procedures that allow researchers to record and stimulate within specific human brain structures. Investigations within the human brain offer revolutionary opportunities for studying how the human brain functions but are often constrained by the availability of resources and the limited number of patients undergoing these types of procedures. This funding opportunity supports innovative, exploratory research that is only possible through direct access to the brain to better understand various processes, including how the human brain senses, perceives, understands, generates language, and activates movements. Within the NIDCD scientific mission areas — spanning speech and language, auditory and vestibular function, and smell and taste — lies the rich potential for understanding the cellular and neural basis of behavior. Additionally, the program has a specific interest in supporting diverse, multi-disciplinary teams consisting of clinicians, scientists, device engineers, data/computational scientists, regulatory specialists, and ethics specialists. Awardees will participate in a working group to develop standards of practice (including neuroethical considerations), and collect, aggregate, and standardize data for sharing with the wider scientific community. NIDCD hopes these early studies will lay the groundwork for future intracranial research to address the disorders within NIDCD’s mission and across diverse areas of neuroscience.
Budget Policy: The FY 2025 President’s Budget request for the Hearing and Balance Program is $243.3 million, an increase of $0.6 million or 0.3 percent compared with the FY 2023 Final level.
Taste and Smell Program
NIDCD supports studies of the chemical senses — taste (gustation), smell (olfaction), and chemesthesis (chemically provoked irritation) — to enhance our understanding of how gustatory and olfactory cues from the external environment are processed and how human chemosensory disorders can be diagnosed and treated. NIDCD places a high priority on research aimed at identifying the underlying mechanisms important for both normal development of taste and smell and for developing treatment and prevention strategies for taste and smell disorders.
Food choice has a profound impact on our overall health. NIDCD is supporting research to understand how what we taste changes our brain to influence adult food choices and achieve progress to enhance nutrition.22 The gustatory cortex (GC) in the brain specializes in taste-related functions, such as anticipating taste and identifying safe and spoiled foods. Using a mouse model, NIDCD-supported researchers found evidence that neural circuits in the GC change based on early taste experience, thus establishing sweet preference. They identified a critical period during early life when sweet preference is established and described how early taste experiences influence GC circuits to maintain this preference in adult mice. These findings highlight the importance of early taste experiences both for adult taste preferences and for establishing normal taste circuitry in the developing GC.
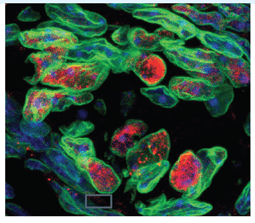
The World Health Organization estimates that vector-borne illnesses account for more than 17 percent of all infectious diseases worldwide and are responsible for more than 700,000 deaths annually.23 Mosquitos use their sense of smell to identify the source of their next blood meal. The Aedes aegypti mosquitos prefer to feed on humans over animals, thus spreading human bloodborne diseases such as encephalitis, malaria, dengue, West Nile, and Zika. NIDCD-supported investigators are working to determine how the insects preferentially target humans.24
They studied odor signaling in the clusters of nerve cell synapses within the mosquito brain, called glomeruli, that receive input from olfactory receptors. The team identified a specific glomerulus that is strongly activated by human odor but not by animal odor. Their experiments determined that human odor is enriched in long-chain aldehydes, most likely derived from sebum, an oily skin protectant secreted into hair follicles. The long-chain aldehydes specifically activate the human-responsive mosquito glomerulus, helping the mosquito brain distinguish a human scent from an animal scent, and stimulate female mosquitos to target the human odor source for their blood meal. Scientists now hope to use this information to develop new ways to prevent mosquitos from biting humans and spreading serious diseases.
Budget Policy: The FY 2025 President’s Budget request for the Taste and Smell Program is $58.0 million, an increase of $0.2 million or 0.3 percent compared with the FY 2023 Final level.
Voice, Speech, and Language Program
Disorders involving voice, speech, or language can have an overwhelming effect on an individual’s health and quality of life. These disorders affect people of all ages with or without hearing impairment, including children with autism, those who stutter, and adults with acquired communication disorders. Voice, speech, and language disorders also come at a significant cost.25 The cost to society of laryngeal disorders alone is estimated at $11 billion annually due to work-related disability, lost productivity, and direct health care cost. By the first grade, roughly five percent of children have noticeable speech disorders.26 In children, delayed speech and language acquisition or impairment are often significant predictors of future academic, social, vocational, and adaptive outcomes.
Autism spectrum disorder (ASD) is a complex developmental disorder that affects behavior, communication, and social interaction. About 1 in 36 children are identified with ASD in the United States27, and approximately 25 percent of children with ASD are minimally verbal or non-speaking. Early identification and intervention can improve overall social and emotional outcomes. In 2023, NIDCD sponsored a webinar to foster the development of critical research studies addressing the varying communication needs and abilities of this population. The discussants represented a wide range of backgrounds and perspectives and included scientists, advocates, and individuals with autism. From this workshop, NIDCD published a Notice of Special Interest to promote language and communication research in minimally verbal or non-speaking individuals with autism.28 The Notice encourages research to evaluate and tailor existing interventions, develop novel interventions, develop and apply new research designs and methods to intervention efforts, and identify meaningful outcome measures.
Essential tremor (previously also called benign essential tremor or familial tremor) is one of the most common movement disorders. The key feature is a tremor in both hands and arms, but a person’s voice is also affected. Although the tremor can start at any age, it most often first appears during adolescence or in middle age (between ages 40 and 50). It can be mild and stay mild, or slowly get worse over time. The exact cause of essential tremor is unknown, and finding treatments is a challenge. NIDCD-funded voice researchers tested the use of an FDA-approved drug, sodium oxybate, which is used for excessive daytime sleepiness in children and adults with narcolepsy (a disorder where there is an extreme tendency to fall asleep).29 The researchers found that sodium oxybate targets the same areas in the brain that are suspected to cause the tremors. This open-label study is the first to show that patients with a particular type of essential tremor have an average of 41 percent reduction in their symptoms after a single-dose of sodium oxybate. These findings are an important first step in providing some relief to those with essential tremor of voice.
NIDCD Workshop: Research Needs in Stuttering – Roadblocks and Future Directions
Roughly 3 million Americans experience stuttering, characterized by frequent repetition of words or parts of words that disrupts the smooth flow of speech. Stuttering affects people of all ages. It occurs most often in children between the ages of two and six as they are developing their language skills. While most children outgrow stuttering, 25 percent will continue to stutter. For those with persistent stuttering, it is a lifelong communication disorder that affects a person’s quality of life and interpersonal relationships. Stuttering can negatively influence job performance and opportunities, and treatment can come at a high financial cost.
In 2023, NIDCD hosted a workshop for researchers, clinicians, and potential future grant applicants with scientific expertise in stuttering. Participants discussed the biological basis, indicators of persist stuttering and recovery, speech and movement control, cognitive and social factors, and treatment of stuttering. The goal of the workshop was to identify the opportunities and next steps for the scientific community with respect to these areas.
Budget Policy: The FY 2025 President’s Budget request for the Voice, Speech and Language Program is $151.1 million, an increase of $0.4 million or 0.3 percent compared with the FY 2023 Final level.
Intramural Research Program
The NIDCD Intramural Research Program (IRP) conducts basic and clinical research in human communication. In the past few years, the IRP program has made important changes including the addition of new programs.
NIDCD recently hired a new Clinical Director. The Clinical Director oversees NIDCD’s clinical and translational research program conducted in the NIH Clinical Center, a world-class research hospital located on the NIH campus in Bethesda, Maryland. NIDCD’s clinical program fosters interaction to support pre-clinical, translational, and clinical studies aimed at developing novel diagnostic and therapeutic strategies for disorders affecting hearing, balance, taste, smell, voice, speech, and language. Under this new leadership, the program will provide clinical training opportunities for future clinician-scientists, including physicians who are engaged in cutting-edge, translational research through NIDCD’s Otolaryngology Surgeon-Scientist Program.30 The Clinical Director will also head NIDCD’s new Sinonasal and Olfaction Program where a multidisciplinary team will explore basic science discoveries that have the potential to advance taste and smell treatments for patients.31
In 2023, NIDCD established a new Neurotology Branch. The branch will oversee clinical trials to identify promising new pharmacologic, biologic, gene therapy, and surgical procedures to advance treatments for hearing impairment, tinnitus, and balance disorders. Focus areas include the molecular pathways that direct hair cell (sensory cells in the inner ear) development and survival, sex differences in hearing and acquired hearing loss, and innovative tools for sharing, visualization, and analyzing data. Bringing this expertise to the NIDCD intramural program affords the opportunity for high-risk, high-reward research and acceleration of translating emerging basic science discoveries into impactful advances for hearing and balance disorders.
NIDCD intramural scientists are also working to identify therapeutic targets and novel treatments for sudden hearing loss and hearing instability disorders, including Ménière’s disease. Corticosteroids are the current standard of care for these types of inner ear diseases. However, complete recovery is rare, and results vary from person to person. To address this clinical need, an NIDCD intramural research team used a data-science approach to cross-reference steroid-responsive gene targets with FDA approved medications.32 The researchers identified 42 medications that have been shown to interact with these gene targets. The findings provide the basis for future clinical trials utilizing repurposed drugs that have demonstrated safety and tolerability in humans. Repurposing drugs provides an opportunity to speed development and testing of therapies available to individuals with few effective treatment options to restore hearing.
Budget Policy: The FY 2025 President’s Budget request for the Intramural Research Program is $56.7 million, an increase of $0.3 million or 0.6 percent compared with the FY 2023 Final level.
Research Management and Support (RMS) Program
NIDCD RMS activities provide administrative, budgetary, logistical, and scientific support in the review, award, and monitoring of research grants, training awards, and research and development contracts. RMS functions also include strategic planning, coordination, and evaluation of the Institute’s programs, regulatory compliance, and international coordination. NIDCD administrative and program staff liaise with other Federal agencies, Congress, and the public to provide program, policy, health information, and scientific advances. The Institute currently supports approximately 1,400 research grants, training awards, and Research & Development contracts.

Enhancing diversity, equity, inclusion, and accessibility within NIDCD’s workforce is a major priority. With leadership from NIDCD’s first Chief Diversity Officer, the Institute is cultivating a growth mindset that seeks and values diverse perspectives. NIDCD has developed a comprehensive plan to advance racial and ethnic equity for NIDCD employees. With the participation and collaboration with all levels of the NIDCD workforce, this plan includes expanding the awareness of cultural issues that impact the employee experience in the workplace through training and education on a wide range of topics, such as inclusive pronoun uses, ableism, biases against certain dialects, and structural racism. To expand on practices to support fair and consistent hiring practices, NIDCD has created step-by-step guidance on reducing bias in recruitment and a policy utilizing search committees for specific leadership positions. These efforts will focus on ensuring that hiring managers and selecting officials receive resources to support their ability to recognize the merits of all candidates.
Budget Policy: The FY 2025 President’s Budget request for RMS is $26.8 million, an increase of $0.1 million or 0.2 percent compared with the FY 2023 Final level.
| Fiscal Year | Budget Estimate to Congress | House Allowance | Senate Allowance | Appropriation |
|---|---|---|---|---|
| 2016 | $416,241,000 | $412,366,000 | $424,860,000 | $423,031,000 |
| Rescission | $0 | |||
| 20171 | $422,936,000 | $434,126,000 | $441,778,000 | $436,875,000 |
| Rescission | $0 | |||
| 2018 | $325,846,000 | $443,624,000 | $451,768,000 | $459,974,000 |
| Rescission | $0 | |||
| 2019 | $423,992,000 | $465,467,000 | $474,653,000 | $474,404,000 |
| Rescission | $0 | |||
| 2020 | $408,358,000 | $497,590,000 | $500,270,000 | $490,692,000 |
| Rescission | $0 | |||
| 2021 | $446,397,000 | $494,912,000 | $506,670,000 | $498,076,000 |
| Rescission | $0 | |||
| 2022 | $511,792,000 | $522,758,000 | $511,280,000 | $514,885,000 |
| Rescission | $0 | |||
| 2023 | $508,704,000 | $531,136,000 | $530,847,000 | $534,333,000 |
| Rescission | $0 | |||
| 2024 | $534,330,000 | $534,333,000 | $534,333,000 | $534,333,000 |
| Rescission | $0 | |||
| 2025 | $535,929,000 | |||
| 1 Budget Estimate to Congress includes mandatory financing. | ||||
Authorizing Legislation
| (Dollars in Thousands) | |||
|---|---|---|---|
| Source of Funding | FY 2023 Final | FY 2024 CR | FY 2025 President's Budget |
| Appropriation | $534,333 | $534,333 | $535,929 |
| Mandatory Appropriation: (non-add) | |||
| Type 1 Diabetes | ($0) | ($0) | ($0) |
| Other Mandatory financing | ($0) | ($0) | ($0) |
| Subtotal, adjusted appropriation | $534,333 | $534,333 | $535,929 |
| OAR HIV/AIDS Transfers | -$3 | $0 | $0 |
| Subtotal, adjusted budget authority | $534,330 | $534,333 | $535,929 |
| Unobligated balance, start of year | $0 | $0 | $0 |
| Unobligated balance, end of year (carryover) | $0 | $0 | $0 |
| Subtotal, adjusted budget authority | $534,330 | $534,333 | $535,929 |
| Unobligated balance lapsing | -$3 | $0 | $0 |
| Total obligations | $534,327 | $534,333 | $535,929 |
| 1 Excludes the following amounts (in thousands) for reimbursable activities carried out by this account: FY 2023 – $850 FY 2024 – $856 FY 2025 – $856 | |||
| (Dollars in Thousands) | ||||
|---|---|---|---|---|
| FY 2024 CR | FY 2025 President's Budget | |||
| Total compensable workyears: | ||||
| Full-time equivalent | 140 | 140 | ||
| Full-time equivalent of overtime and holiday hours | 0 | 0 | ||
| Average ES salary | $222 | $226 | ||
| Average GM/GS grade | 12.9 | 12.9 | ||
| Average GM/GS salary | $147 | $150 | ||
| Average salary, Commissioned Corps (42 U.S.C. 207) | $171 | $178 | ||
| Average salary of ungraded positions | $127 | $130 | ||
| OBJECT CLASSES | FY 2024 CR | FY 2025 President's Budget | ||
| Personnel Compensation | ||||
| 11.1 | Full-Time Permanent | $15,284 | $15,711 | |
| 11.3 | Other Than Full-Time Permanent | $5,564 | $5,720 | |
| 11.5 | Other Personnel Compensation | $808 | $831 | |
| 11.7 | Military Personnel | $205 | $215 | |
| 11.8 | Special Personnel Services Payments | $2,528 | $2,598 | |
| 11.9 | Subtotal Personnel Compensation | $24,389 | $25,076 | |
| 12.1 | Civilian Personnel Benefits | $7,962 | $8,228 | |
| 12.2 | Military Personnel Benefits | $38 | $40 | |
| 13.0 | Benefits to Former Personnel | $0 | $0 | |
| Subtotal Pay Costs | $32,388 | $33,343 | ||
| 21.0 | Travel & Transportation of Persons | $311 | $293 | |
| 22.0 | Transportation of Things | $100 | $103 | |
| 23.1 | Rental Payments to GSA | $0 | $0 | |
| 23.2 | Rental Payments to Others | $0 | $0 | |
| 23.3 | Communications, Utilities & Misc. Charges | $8 | $8 | |
| 24.0 | Printing & Reproduction | $4 | $4 | |
| 25.1 | Consulting Services | $13,078 | $13,164 | |
| 25.2 | Other Services | $11,513 | $11,016 | |
| 25.3 | Purchase of Goods and Services from Government Accounts | $42,077 | $42,476 | |
| 25.4 | Operation & Maintenance of Facilities | $254 | $254 | |
| 25.5 | R&D Contracts | $3,052 | $3,119 | |
| 25.6 | Medical Care | $470 | $488 | |
| 25.7 | Operation & Maintenance of Equipment | $1,549 | $1,434 | |
| 25.8 | Subsistence & Support of Persons | $0 | $0 | |
| 25.0 | Subtotal Other Contractual Services | $71,993 | $71,952 | |
| 26.0 | Supplies & Materials | $2,352 | $2,054 | |
| 31.0 | Equipment | $2,289 | $1,989 | |
| 32.0 | Land and Structures | $0 | $0 | |
| 33.0 | Investments & Loans | $0 | $0 | |
| 41.0 | Grants, Subsidies & Contributions | $424,883 | $426,179 | |
| 42.0 | Insurance Claims & Indemnities | $0 | $0 | |
| 43.0 | Interest & Dividends | $4 | $4 | |
| 44.0 | Refunds | $0 | $0 | |
| Subtotal Non-Pay Costs | $501,945 | $502,586 | ||
| Total Budget Authority by Object Class | $534,333 | $535,929 | ||
| 1 Includes FTEs whose payroll obligations are supported by the NIH Common Fund. | ||||
| (Dollars in Thousands) | |||
|---|---|---|---|
| Object Classes | FY 2024 CR | FY 2025 President's Budget | |
| Personnel Compensation | |||
| Full-Time Permanent (11.1) | $15,284 | $15,711 | |
| Other Than Full-Time Permanent (11.3) | $5,564 | $5,720 | |
| Other Personnel Compensation (11.5) | $808 | $831 | |
| Military Personnel (11.7) | $205 | $215 | |
| Special Personnel Services Payments (11.8) | $2,528 | $2,598 | |
| Subtotal, Personnel Compensation (11.9) | $24,389 | $25,076 | |
| Civilian Personnel Benefits (12.1) | $7,962 | $8,228 | |
| Military Personnel Benefits (12.2) | $38 | $40 | |
| Benefits to Former Personnel (13.0) | $0 | $0 | |
| Subtotal Pay Costs | $32,388 | $33,343 | |
| Travel & Transportation of Persons (21.0) | $311 | $293 | |
| Transportation of Things (22.0) | $100 | $103 | |
| Rental Payments to Others (23.2) | $0 | $0 | |
| Communications, Utilities & Misc. Charges (23.3) | $8 | $8 | |
| Printing & Reproduction (24.0) | $4 | $4 | |
| Other Contractual Services | |||
| Consultant Services (25.1) | $11,691 | $12,010 | |
| Other Services (25.2) | $11,513 | $11,016 | |
| Purchases of Goods and Services from Government Accounts (25.3) | $23,936 | $24,230 | |
| Operation & Maintenance of Facilities (25.4) | $254 | $254 | |
| Operation & Maintenance of Equipment (25.7) | $1,549 | $1,434 | |
| Subsistence & Support of Persons (25.8) | $0 | $0 | |
| Subtotal Other Contractual Services | $48,943 | $48,944 | |
| Supplies & Materials (26.0) | $2,352 | $2,054 | |
| Subtotal Non-Pay Costs | $51,719 | $51,406 | |
| Total Administrative Costs | $84,107 | $84,749 | |
| Office | FY 2023 Final | FY 2024 CR | FY 2025 President's Budget | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Civilian | Military | Total | Civilian | Military | Total | Civilian | Military | Total | |
| Division of Extramural Activities | |||||||||
| Direct: | 18 | - | 18 | 18 | - | 18 | 18 | - | 18 |
| Total: | 18 | - | 18 | 18 | - | 18 | 18 | - | 18 |
| Office of the Director | |||||||||
| Direct: | 3 | - | 3 | 3 | - | 3 | 3 | - | 3 |
| Total: | 3 | - | 3 | 3 | - | 3 | 3 | - | 3 |
| Division of Intramural Research Program | |||||||||
| Direct: | 57 | 1 | 58 | 63 | 1 | 64 | 63 | 1 | 64 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 57 | 1 | 58 | 63 | 1 | 64 | 63 | 1 | 64 |
| Division of Scientific Programs | |||||||||
| Direct: | 19 | - | 19 | 19 | - | 19 | 19 | - | 19 |
| Total: | 19 | - | 19 | 19 | - | 19 | 19 | - | 19 |
| Office of Administration | |||||||||
| Direct: | 36 | - | 36 | 36 | - | 36 | 36 | - | 36 |
| Total: | 36 | - | 36 | 36 | - | 36 | 36 | - | 36 |
| Total | 133 | 1 | 134 | 139 | 1 | 140 | 139 | 1 | 140 |
| Includes FTEs whose payroll obligations are supported by the NIH Common Fund. | |||||||||
| FTEs supported by funds from Cooperative Research and Development Agreements. | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| FISCAL YEAR | Average GS Grade | ||||||||
| 2021 | 12.6 | ||||||||
| 2022 | 12.8 | ||||||||
| 2023 | 12.9 | ||||||||
| 2024 | 12.9 | ||||||||
| 2025 | 12.9 | ||||||||
| GRADE | FY 2023 Final | FY 2024 CR | FY 2025 President's Budget |
|---|---|---|---|
| Total, ES Positions | 1 | 1 | 1 |
| Total, ES Salary | $212,100 | $221,900 | $226,338 |
| General Schedule | |||
| GM/GS-15 | 27 | 28 | 28 |
| GM/GS-14 | 20 | 20 | 20 |
| GM/GS-13 | 31 | 32 | 32 |
| GS-12 | 17 | 18 | 18 |
| GS-11 | 3 | 3 | 3 |
| GS-10 | 0 | 0 | 0 |
| GS-9 | 3 | 4 | 4 |
| GS-8 | 3 | 3 | 3 |
| GS-7 | 1 | 1 | 1 |
| GS-6 | 0 | 0 | 0 |
| GS-5 | 1 | 1 | 1 |
| GS-4 | 0 | 0 | 0 |
| GS-3 | 0 | 0 | 0 |
| GS-2 | 1 | 1 | 1 |
| GS-1 | 0 | 0 | 0 |
| Subtotal | 107 | 111 | 111 |
| Commissioned Corps (42 U.S.C. 207) | |||
| Assistant Surgeon General | 0 | 0 | 0 |
| Director Grade | 0 | 0 | 0 |
| Senior Grade | 1 | 1 | 1 |
| Full Grade | 0 | 0 | 0 |
| Senior Assistant Grade | 0 | 0 | 0 |
| Assistant Grade | 0 | 0 | 0 |
| Junior Assistant | 0 | 0 | 0 |
| Subtotal | 1 | 1 | 1 |
| Ungraded | 51 | 52 | 52 |
| Total permanent positions | 109 | 115 | 115 |
| Total positions, end of year | 160 | 165 | 165 |
| Total full-time equivalent (FTE) employment, end of year | 134 | 140 | 140 |
| Average ES salary | $212,100 | $221,900 | $226,338 |
| Average GM/GS grade | 12.9 | 12.9 | 12.9 |
| Average GM/GS salary | $140,141 | $147,428 | $150,377 |
| 1 Includes FTEs whose payroll obligations are supported by the NIH Common Fund. | |||
[30] nidcd.nih.gov/training/otolaryngology-surgeon-scientist
*Note: PDF files require a viewer such as the free Adobe Reader.

