October 8, 2020
Virtual Workshop
Workshop Summary
On this page:
- Introduction
- OM research: Past, present, future
- Epidemiology, public health, and disease burden
- State of treatment/prevention
- Research barriers, successes, and translation
- Developmental impact and lifespan sequelae
- Workforce pipeline and training
- Summary and conclusions
Introduction
On October 8, 2020, the National Institute on Deafness and Other Communication Disorders (NIDCD) convened a group of scientific experts online for the NIDCD Workshop in Otitis Media (OM) in Early Childhood. The purpose of the virtual workshop was to collect scientific input on ways to advance research on otitis media (middle ear infections). Given the public health burden of OM in the U.S. and globally, the goal was to identify scientific strategies to accelerate the transition from the basic discovery phase to disease prevention and therapies. The panel addressed the decline in OM research supported by the NIDCD as well as the investigator pipeline.
To help facilitate discussion, the following broad general topic areas were identified:
- OM research: past, present, and future
- Epidemiology, public health, and disease burden
- State of treatment/prevention
- Research barriers, successes, and translation
- Developmental impact and lifespan sequelae
- Workforce pipeline and training
Prior to the workshop, subpanels were formed based on the topic areas. The subpanels then met periodically to address the assigned topic area. Each subpanel prepared a report for presentation at the workshop. The scientific experts’ focus was on the science. They have not had nor will they have any role in formulating, recommending, or determining any funding initiatives.
OM research: Past, present, and future
Statement of the issues
The objectives of this section are to identify key topics/studies that influenced past and present OM research, and to identify potential future directions in research on OM pathogenesis and improvements in diagnosis, treatment, and prevention. Past OM research was either primarily descriptive in nature or focused on treatment outcomes. Present studies are more mechanistic and seek to understand the pathogenesis of the disease at the cellular and molecular level, identify vaccine candidates, and develop novel therapeutic approaches. Future research should continue efforts to understand OM using evolving and innovative methods, especially focused on OM chronicity and improvements to prevention and treatment. Future studies are briefly outlined below and treated in detail in the subsequent sections.
- Past studies
- Basic anatomy and physiology of the middle ear (ME) during OM.
- Structure and function of the eustachian tube (ET).
- Species and characteristics of bacteria and viruses in OM.
- Cellular and humoral immune response of the ME during OM.
- Comparative effects of antibiotics.
- Effects of adenoidectomy and tonsillectomy on OM.
- Effectiveness of ventilation tubes.
- Watchful waiting versus antibiotic therapy.
- Present studies
- Identification and characterization of biofilm in OM.
- Microbial gene analysis for determining genome content of pathogens causing OM.
- Characterization and identification of effective vaccine candidates [Streptococcus pneumoniae (Spn), non-typeable Haemophilus influenzae (NTHi), and Moraxella catarrhalis (Mcat)].
- Elucidating key cell signaling pathways and gene and protein expression patterns of the host immune responses in OM pathogenesis using multiple approaches including microarray, RNA-Seq, and mass spectrometry for omics analysis.
- Development of acute and chronic OM animal models using knockout and mutant mice to identify genes critical to OM pathogenesis and recovery.
- Identification of processes that drive mucosal hyperplasia and mucus production in OM.
- Genomic sequence of the chinchilla has advanced proteomic and metabolomic studies in this animal model.
- Development of noninvasive drug delivery systems for ototopical administration of therapeutic agents, including antibiotics and anti-inflammatory agents across the eardrum (e.g., tympanic membrane-transiting peptides, hydrogels with chemical permeation enhancers, magnetic particles).
- Effects of pneumococcal vaccines on OM prevalence and characteristics.
- Molecular genetic studies in humans to identify key genes: genome-wide association studies (GWAS), association studies of candidate genes.
- Future studies
- Determine the true incidence and burden of OM worldwide, including population-specific differences.
- Improve understanding of molecular mechanisms underlying OM chronicity.
- Define innate and adaptive immune regulatory mechanisms for effective ME protection by vaccines and for identification of new therapeutic targets.
- Improve animal models of acute and chronic OM such as humanized animal models and ME-specific knock-out and knock-in mutations, including use of CRISPR-Cas9.
- Omics data mining (human, animal, and single cell): identify the key therapeutic targets or biomarkers based on transcriptome and proteome studies using human OM samples. Such approaches are also critical for identifying new protein-protein interactions, post-translational modifications, and transcriptome-proteome correlations (integrative omics studies).
- Otitis-prone children often have a pronounced delay in the development of immune responses compared with non-otitis-prone children.
- Determine if this delay occurs primarily as a result of an early infection and/or environmental responses that attenuate/tolerize the immune response, possibly via epigenetic changes.
- Determine if this delay is primarily genetic in nature.
- Additional areas where we need to advance include accelerated treatment options, animal models of ET dysfunction, advanced diagnostics of bacterial infection, ME effusion, bacterial biofilms, and viruses.
- Relating bacterial factors to disease and immunity, to define bacterial-host interactions to the molecular level:
- Bacteria-focused:
Identifying/characterizing bacterial factors involved in:- Colonizing respiratory tract and ascending ET: potential vaccine targets.
- Attachment/biofilm: potential therapeutic targets.
- Immunomodulation: potential vaccine and/or immunostimulatory-therapeutics (individual proteins, secretion systems, polysaccharides, lipids, glycans, TLR agonists and/or antagonists, etc.).
- Host-focused:
Identifying host features that impact OM:- Host immune functions mediating control/clearance of infection.
- Physical barriers: ET, cilia, mucus, secretions.
- Mucosal hyperplasia.
- Innate immunity: molecules: receptors, anti-microbial peptides, complement, etc.; inflammatory cells: macrophages, PMNs, eosinophils, etc.
- Adaptive immunity: humoral (B cell): IgA, IgG; cellular (T cell): Th1, Th2, Th17, Tre, etc.
- Bacterial-host interactions:
- Manipulate both bacteria and host during OM, to define immunological targets of bacterial factors and prevent or reverse the disease process.
- Bacteria-focused:
Epidemiology, public health, and disease burden
Statement of the issues
OM is a significant health and economic burden in developed countries, especially for underserved populations. In the developing world, OM qualifies as a serious health crisis due to lack of adequate and advanced medical care, leading to high levels of lifelong morbidity and unacceptable childhood mortality. Current data on the status of OM is lacking. Epidemiologic studies are needed to identify the true magnitude of the problem and focus on identifying children who are at highest risk for recurrent, persistent, and suppurative disease with the goal of identifying modifiable risk factors.
Key research questions:
- What is the true burden of otitis media worldwide?
- What is the impact of OM on hearing and language development, both in developed and developing countries?
- What are the effects of sequelae (e.g., perforations, chronic suppurative OM) on quality of life?
- What are the key genetic, behavioral, and environmental risk factors that determine whether a child is/becomes prone to OM?
- Which, if any, of these risk factors can be modified and how?
- What are novel strategies for prevention?
- The epidemiology of OM is changing: Data suggest that acute OM incidence is decreasing and chronic OM is increasing globally. The shifts in pathogens, vaccines, and vaccine coverage provide continuously moving targets that require ongoing evaluation and research efforts. New bacterial taxa and viruses have been linked to OM, but their role in pathogenesis, if any, is unclear. Data from clinical and population-based studies can be used to inform mechanistic work in laboratory and/or animal models.
- Research needs:
- Updated incidence and prevalence rates by OM definition (acute OM, chronic OM with effusion or COME, suppurative OM, complications) and by pathogen.
- Potential translational studies to fill the gap:
- Natural history study of OM involving large birth cohort; multi-center study with infants followed for up to five years; infections and symptoms tracked, and samples (e.g., nasal/nasopharyngeal swabs, serum, stool) collected.
- Research needs:
- Health inequities exist for OM and related complications: There is considerable country to country and population heterogeneity in OM incidence. There are sociocultural differences in opinions about OM as an illness as well as differences in access to care and resources across international settings. Moreover, the age distribution of OM and associated complications differs across settings (e.g., for mastoiditis). The burden of chronic suppurative otitis media (CSOM) is especially high in low-income countries and under-resourced communities within the U.S.
- Research needs:
- Epidemiologic studies in different racial and ethnic groups (e.g., indigenous populations with high OM prevalence).
- Examples of translational studies that could fill the gap:
- Prevalence studies of severe outcomes (e.g., chronic suppurative OM, undertreated OM and its effect on learning and language acquisition) in diverse and/or disadvantaged populations; work must be done in a manner that is culturally sensitive.
- Linking quick ear exams to times when children are being vaccinated; focus on draining ears in middle- and low-income countries.
- Research needs:
- The relative role of behavior, genetics, and the environment in recurrent and persistent OM is unknown: Moving forward, the focus should be on children with recurrent and persistent OM. There are large differences between children in immune maturation; does early infection cause delays in immune maturation that influence subsequent susceptibility to OM, or is early susceptibility a marker of a process that is fundamentally due to genetics?
- Research needs:
- Prospective population-based studies in rural and urban populations.
- Examples of translational studies that could fill the gap:
- Birth cohort study; samples collected for microbiome analyses; comparison could include who does and does not develop early/recurrent OM, and/or immune responses and their impact on the microbiome and/or vice versa.
- Research needs:
- The validity of data in many published studies is questionable: There are concerns with the use of medical records and large databases. Standardized disease definitions, diagnostic criteria, outcome measures, and methodologies are needed so that data can be pooled and compared across studies. Ear taps are no longer/rarely done, and it is difficult to obtain representative collections of OM pathogens from the site of infection.
- Research needs:
- Better/standardized disease definitions, outcome measures, and methodologies.
- Biomarkers for otitis media and algorithms that are predictive of microbiologic and clinical outcomes.
- Pathogens collected from the site of infection.
- Examples of translational studies that could fill the gap:
- Research or working groups to identify best practices and novel study designs.
- Research needs:
State of treatment/prevention
Statement of the issues
Treatment for OM, consisting primarily of systemic antibiotics and the insertion of ventilation tubes, has changed little for decades, and new therapies are clearly needed. Prevention consists primarily of the pneumococcal conjugate vaccine (PCV), which covers only 13 strains and has had modest effects on OM incidence due to replacement by other bacterial species and Spn strains. Pathogen replacement remains an evolving process. More effective OM prevention is also needed. Finally, the reasons that some children are otitis-prone and others OM-resistant remain poorly understood and may be key to treatment and prevention.
- Inability to deliver drugs directly to the middle ear to advance treatment of OM: there are many challenges to direct delivery, both anatomical and physiological, yet multiple advantages.
- Antibiotics do not affect biofilms, leading to recurrent/persistent disease and tube insertion with associated risks.
- Continued development of trans- or intra-tympanic delivery approaches and novel therapeutics to both limit systemic exposure to antibiotics and enable delivery of biofilm-active/regressing agents.
- Continued identification and development of bioactive peptides, bacteriophage, and multiple other agents for delivery via various means (e.g., gels, tympanic membrane penetration enhancers, peptides, magnetically charged agents, etc.).
- Development of new therapeutic agents to enhance innate immunity and host defense; suppress uncontrolled inflammation and mucus production; repair tissue; and speed resolution of inflammation, leading to improved treatment for otitis media.
- No effective long-term medical therapy exists to promote clearance of ME fluid, impeding treatment: “Glue ear” (chronic OT with effusion, or COME) is the most common reason for surgical procedures in the U.S. Mitigating the viscosity of this tenacious fluid is an obvious therapeutic strategy. Due to the poor understanding of the molecular and physicochemical aspects of the fluid, technical difficulties working with collected samples, limitations in local drug delivery, lack of simple animal models for the study of “non-infectious” COME fluid, and an only perfunctory immunological elucidation of mucin glycoprotein function, these therapeutic strategies have not been fruitful. The primary goal is to prevent conductive hearing loss that results in the need for tympanostomy tube surgery; the secondary goal is to prevent recurrence.
The following were offered as strategies to address this obstacle:- Need for identification and development of good models/sources of human mucus.
- Need for an animal model of glue ear.
- Trans- or intra-tympanic delivery of enzymatic agents, mucolytics, deoxyribonuclease (DNAse), etc., should be tested to mitigate ME fluid viscosity.
Inability to identify children at high risk for recurrent and persistent disease impedes efforts at prevention: The majority of high-risk children declare with early onset of disease. Prevention of disease in this age group has relied on herd immunity as a benefit of broad usage of PCVs, but limited coverage is conferred by PCVs, there is no vaccine for NTHi, and to date, maternal immunization has not proven to be successful. Once disease develops in high-risk children, no vaccine has been demonstrated to prevent further disease, as recurrent OM is due to multiple pathogens, and current immune prevention strategies are limited to 13 of 90+ pneumococcal serotypes.
- Does treatment improve outcome in the long term compared to watchful waiting?
- Lack of understanding of criteria to identify children at high risk of recurrent and/or persistent OM.
- Lack of specific markers (i.e., lab tests, genetic profiles) for children at high risk of recurrent and/or persistent OM.
- Development of approaches to better predict this subset of children would permit early detection and intervention, which is expected to mitigate progression to chronic/recurrent disease.
The following were offered as strategies to address this obstacle:- Studies are needed to determine if high risk is due to eustachian tube-related dysfunction, because the first incidence causes damage that predisposes to recurrent OM or both?
- Does early OM lead to immune tolerance? Are there epigenetic effects?
- Expanded investigation and analysis of the early microbiome in infants with early-onset OM in comparison to those without would be of value and could identify high-risk infants.
- Research is needed to develop methods to alter the nasopharyngeal (NP) microbiome via delivery of pro- or pre-biotics and/or seeding with flora associated with non-high-risk children (e.g., alpha-hemolytic Streptococcus and others).
- A potential additional benefit could be gaining the understanding that the NP microbiome (as shown for the gut microbiome) “educates” the immune system of the respiratory tract, including the ME.
- Inability to prevent biofilm development in the ME or induce its regression or eradication impedes efforts at both prevention and treatment: Abundant data support the significant role of bacterial biofilms in the pathogenesis, chronicity, and recurrence of OM and recalcitrance to treatment/eradication.
The following were offered as strategies to address this obstacle:- Continued work on the development and validation (both in vitro and in vivo) of different strategies to either prevent biofilm development or disrupt them once established.
- Continued work to identify biofilm-targeted approaches (both therapeutic and preventive) by exploring the constituents of the biofilm matrix, aspects of bacterial biology that are unique to biofilm residence, quorum signaling, metabolism, specific bacterial surface, or expressed proteins as potential targets.
- Development of safe ways to deliver biofilm-targeted agents across the tympanic membrane would confer a significant and long-lasting impact on the field.
- Research on polymicrobial biofilms is needed as a better surrogate for natural OM.
- Lack of clinical trials for prevention of OM due to NTHi or Mcat and the unfounded perception that “OM is not much of a problem anymore” because of broad use of PCVs: Greater attention is paid to OM due to Spn because of its acute and highly symptomatic nature. However, OM due to NTHi or Mcat is now more prevalent, and while less symptomatic, confers the same issues of morbidity, early onset, potential for development of multiple sequelae, risk of need for ventilation tube insertion, contribution to antibiotic resistance, etc. Our collective goal should be to prevent ALL OM, even “mild” OM. Despite the identification and often extensive pre-clinical validation of viable vaccine candidates for NTHi or Mcat, there has been no forward progress to clinical trials.
The following were offered as strategies to address this obstacle:- Need for a comprehensive report on the social, financial, and epidemiological implications of OM—including its role in driving global antimicrobial resistance—to foster greater recognition among stakeholders as to the broader impact of OM.
- Develop non-culture-based methods to more accurately detect OM caused by NTHi and Mcat.
- Promote/incentivize public-private partnerships and broaden the discussion of the global impact of OM to include associated extensive morbidity and reduced quality of life; tremendous socioeconomic burden; contribution to global antibiotic resistance; and the fact that OM disproportionately affects indigenous and disadvantaged populations. Methods to better share associated risk should be explored.
- Leverage chronic obstructive pulmonary disease (COPD) as a vaccine target.
- Develop polyvalent vaccines for ME bacterial and viral infections, including polymicrobial infections.
- Any species-wide vaccine could affect beneficial strains in the nasopharynx.
- Opportunities/areas to leverage outside of the NIDCD:
- Transtympanic delivery, mitigation of viscosity, and development of biofilm-targeted agents: There has been industry interest, and several start-ups are currently seeking venture capital and/or development partners; one transtympanic treatment is currently on the market, establishing an FDA precedent.
- Identification of high-risk infants: Various repositories of NP cultures recovered from high-risk infants exist and could be leveraged for microbiome studies.
- Vaccines for NTHi & Mcat: Hold a planning group to bring together stakeholders including NIDCD, NIAID, NIMHD, FDA, pharma, Gates Foundation, and entities that target antimicrobial resistance, such as CARBX; short talks by WHO to present the global problem, a clinician/surgeon to address severe and early OM as experienced by multiple disadvantaged populations, a speaker to address the vast economic burden of OM, and mechanisms to share risk.
Research barriers, successes, and translation
Statement of the issue
While modest progress has been made in translating basic OM research to therapies, there are major barriers to advancing research findings to the clinic. In order to advance OM prevention and treatment, these barriers need to be identified, and strategies to overcome them must be developed.
- Perception that with broad use of PCVs, “OM is not much of a problem anymore” hinders research:
- Among both grant reviewers and commercial entities, a widespread belief that PCVs have solved the problem of OM needs to be addressed.
- A comprehensive report/statement on the current status as well as the health, epidemiologic, and global burdens of OM is needed to inform stakeholders.
- Lack of clinical trials for prevention of OM due to NTHi or MCat:
- As noted above, despite the identification of several viable vaccine candidates for NTHi or MCat, progress is still needed toward clinical trials for prevention of OM due to these pathogens.
- No human trials for Gram-negative bacteria over 25 years; minimal buy-in from pharmaceutical companies.
- Antimicrobial resistance is a real problem; this point needs to be made in terms of underscoring the importance of vaccines.
- Prevention for chronic obstructive pulmonary disease is needed, given the global morbidity and mortality associated with the disease; this could help underscore the significance of an effective NTHi vaccine.
- The possibility of vaccine trials through NIH should be explored, potentially including NIAID.
- Lack of adequate immunologic animal models for the study of OM:
- Rapid progress in understanding the immunologic aspect of these complex interactions is dependent on the many tools and approaches only available in the mouse model.
- Mouse models need to be better developed to represent chronic OM and better define immune mechanisms that can mediate efficient control/clearance so we can induce them with vaccines or drugs.
- Studies of mucosal immunology of the ME are needed.
- The role of individual leukocyte types in ME immune responses should be evaluated.
- Understanding how mouse models reflect human immune responses, such as via humanized mice, should be explored.
- The strength of current mouse models is not in treatment, but in genetics; treatment options could be explored in this model.
- Immunology in the chinchilla model needs to be better understood.
- Insufficient research into the genetic basis of OM:
- OM is a complex genetic disorder where single-gene methods are inappropriate. Human genome-wide association studies in OM are still relatively few and small.
- Hundreds of thousands of subjects should be acquired to adequately map single nucleotide polymorphisms to phenotypes.
- The International Childhood Disease Alliance (ICDA) studies disease pathophysiology through fine mapping of genes and variants. Given that OM is a common disease, it should be included as a flagship disease in ICDA; NIH outreach?
- Effective phenotyping methods for OM genetic cohorts will be challenging and need to be identified. Tympanostomy rates or parent questionnaires could be adequate proxies.
- National Children’s Health Study could be a source of genetic material if adequately phenotyped.
- DNA from previously phenotyped OM cohorts (Minnesota/Pittsburgh) should be available, although the cohorts are small.
- Murine GWAS, using a genetically well-characterized panel of 100 mouse strains, would allow strict phenotyping and require much smaller numbers.
- Insufficient coordination between research groups:
- Cooperation and coordination between research groups (both within institutions and between institutions) can be a key to progress.
- Establishment of inter-institutional research consortia has been used successfully to advance research in many fields.
- One or more OM consortia would reduce duplication of resources, permit new studies that efficiently integrate different methodologies and approaches, and help to grow the field.
- Challenges/limitations to achieving therapeutic outcomes:
- Need for more cross-discipline studies; link discoveries in pathogenesis with clinical investigations to assess feasibility/outcomes.
- Clinical/scientific community/public perception of need for novel treatments?
- Limitations due to aspects of the animal models, with potential caveats due to dissimilarities to human infection; non-mouse models with few immunological tools have limited the study of immunology in OM.
- Challenges with diagnosis; clinical diagnosis of different OM types (acute, with effusion, chronic, recurrent).
- Developed versus developing countries; susceptibility of disease in populations.
- Cross-discipline; basic/clinical investigator partnerships; clinical perspective on translational potential and clinical impact is often lacking.
- Need for OM consortia (OM partnerships to pool strengths) to help move the field forward.
- Intellectual property and associated challenges, conflict with need to publish.
- Anti-biofilm drugs:
- Need for additional atomic structures (crystallographic or cryogenic electron microscopy) for target molecules associated with the stringent response. RelA/RSH/SpoT/DDK/others for universal in silico molecular docking studies to identify initial “hit” compounds.
- Need for additional protein/enzyme reagents for a range of pathogens for biochemical/biophysical studies.
- Access to an adequate animal model of chronic OM for preclinical trials.
- Development of microbiome-sparing vaccines:
- Need for consortia to perform toxicology, kinetic, preclinical, and clinical trials.
- Need for mechanistic studies of in silico-identified candidate virulence/specific tissue-tropism genes.
- Need for atomic structures (crystallographic or cryo-EM) for identified target molecules to help with epitope identification.
Developmental impact and lifespan sequelae
Statement of the issues
Under-treated chronic, suppurative OM is estimated to cause half of the world’s burden of moderate-to-severe hearing loss (~200 million cases), and ~30,000 annual deaths, primarily in the developing world. The prevalence of OM is ~50% during the first two years, with ~90% of school age children having experienced at least one bout. Furthermore, chronic OM is a prevalent co-morbidity in children with fetal alcohol spectrum disorders (77%), Down syndrome (75%), and craniofacial disorders (60-85%). Suppurative OM is associated with audiometric threshold elevation by ~25 dB (8-53 dB HL) at an age critical to speech and language development.
While clinical trials have mainly targeted severe OM, even mild episodes can be associated with weeks to months of effusion. Non-human studies demonstrate that mild or temporary hearing loss during critical developmental periods, similar to that observed in chronic OM, can cause long-lasting changes to the central nervous system and behavioral skills.
Human studies show that transient childhood OM is a risk factor for delays in language acquisition, deficits in complex auditory processing, and potential learning problems. Human postmortem studies indicate that childhood chronic OM is associated with long- term sensorineural hearing loss in adulthood, suggesting that OM could actually lead to progressive hearing loss during childhood and beyond. Severe hearing loss due to undertreated chronic suppurative OM leads to major social and economic burdens in underserved populations and in many parts of the developing world.
Advances that are likely to have the greatest impact:
- Diagnosis: Research to investigate both causes and methods for increasing the rate of diagnosis (e.g., use of a smartphone app or routine hearing testing by pediatricians) within the first year.
- Determine which factors explain the worldwide OM epidemic (crowding, day care, use of baby formula versus breastfeeding) and whether there are strategies for alleviation.
- Determine whether bacteria (NTHi, Mcat) that cause milder OM than Spn create a "silent" increase of developmental impact and speech and language delays.
- Determine the effect of reduced access to healthcare on OM diagnosis, treatment, and outcome, both within the U.S. and worldwide.
- Determine whether there is a location-specific effect of exposure to bacteria (e.g., rural versus urban environments).
- Determine the genetic underpinnings of OM susceptibility, including in vulnerable populations.
- Recognizing the contributing variables:
- Research to evaluate factors that impact outcomes (e.g., access to healthcare, socioeconomic status, gestational age, birth weight, prenatal alcohol exposure).
- Treatment:
- Investigate means of improving treatments in underserved populations: lower costs, delivery by ancillary medical personnel.
- Vaccine development to prevent more serious disease.
- Long-term consequences:
- Longitudinal human studies are needed to determine the long-term impact of OM in the first years of life, including audiometric and behavioral measures that are monitored into adolescence (spectro-temporal auditory processing, working memory, and language skills).
- Determine the key steps and contributors to the progression from childhood OM to adult sensorineural hearing loss.
- Leveraging current studies:
- "All of Us" research program pipeline: make use of the questionnaire to address some genetic questions.
- Involve The Human Heredity and Health in Africa Initiative (H3Africa) in OM research to evaluate genetic and environmental contributions to severe OM susceptibility.
- Involve the National Children’s Health Study for data mining.
- Basic research:
- Non-human research should identify whether transient mild-to-moderate hearing loss, similar to that experienced during suppurative OM, leads to permanent changes within the central nervous system that are causally linked to behavioral deficits and can be remediated.
Workforce pipeline and training
Statement of the issues
Research on OM in the U.S. is declining. As older researchers leave the field, fewer are being replaced by young faculty. Trainees in OM research units often migrate to other diseases. This is due to a perception that OM is a minor disease that has been “solved” by PCVs, lack of recognition of OM’s impact around the world, and difficulties in obtaining research funding. These perceptions may also negatively impact promotion and tenure decisions for those staying in the field. It is imperative to attract and keep talented scientists within the field of OM research in order for them to develop and maintain competitive careers as OM scientists. We also need to identify scientific research and workforce development strategies to accelerate translation of basic science discoveries to clinical use through modernized research methods and opportunities.
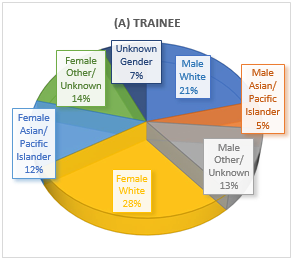
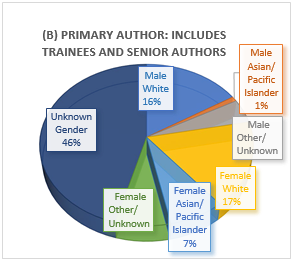
Figure 1. Participation at 2019 ISOM meeting.
Current state and challenges/focus areas
- OM research grant applications scored within the NIDCD payline: Both experienced and early-career scientists are challenged in getting support, including from entities outside the NIDCD. For R01 grants, success rates for OM grants are very low, at 7.7%. On the other hand, for OM-related R21 grants, the success rate is 33.3% (early-career researcher, or ECR, mechanism). For OM, the low success rates may result from failure to attract enough younger principal investigators (PIs) pursuing OM research after older PIs have retired. Experienced PIs, whether through their own submissions as PIs or by guiding less experienced PIs under their purview, are needed to improve the quality of R01 submissions and success rates
- Opportunities for advocating OM research and encouraging trainees and younger faculty to pursue a career in OM research: The International Society of Otitis Media (ISOM) has an integrated research conference providing multiple opportunities for training and professional development. The last ISOM conference was held in Los Angeles in June 2019, with about 105 submitted abstracts by trainees and 60 invited presentations, of which 28 were podium talks presented by trainees (18 female, 10 male). There were also 10 invited trainee moderators (seven female, three male). Figure 1A represents trainees at different levels (graduate, postdoctoral), while Figure 1B shows the gender and ethnic diversity of trainees and established investigators invited to present. The Association for Research in Otolaryngology (ARO) meeting held in San Jose, California, in January 2020 also included an OM-focused symposium in which seven PIs presented their work. In addition, a T32 (training grant) resident presented his work on OM, and seven OM-related posters were presented, mostly by junior researchers. Notably, the posters included work on hearing loss due to OM, suggesting the potential to expand the OM footprint in future ARO meetings.
- Challenges and opportunities in the grant review process: In previous years, OM PIs served on the National Deafness and Other Communication Disorders (NDCD) Advisory Council and in study sections, including as chair. With decreasing numbers of experienced PIs performing OM research, there is a smaller pool of experienced PIs who will review grants and publications and who are actively submitting applications. Among the reviewers who do not perform OM research, there is a higher chance that they do not recognize OM as an important disease with a significant global health care burden, tremendous opportunities for basic science discovery, and significant translational potential. It is unlikely for OM to get a dedicated study section, but there is a possibility to get OM researchers as reviewers in standing study sections. (Of note, applications not discussed or above the payline may have been unsuccessful for reasons not related to their subject matter.) A conscious effort must be made to improve OM applications.
- Long duration of basic science workforce training prior to achieving a stable position to perform OM research: As the median age at which basic science researchers achieve job stability within academia increases, the period during which they are productive as OM researchers shortens. (This is not unique to OM research.) For clinician-scientists, although there is stability from clinical revenue, the pressure to increase clinical revenue can discourage them from dedicating time to basic or clinical OM research.
- Fewer trainees pursuing a research career in OM: The decreasing number of experienced PIs performing OM research feeds into the worsening situation of low numbers of younger faculty and trainees who become interested in OM research. Fewer young researchers who have obtained training in OM continue in the field. They become discouraged and are likely to continue in other research fields with higher success rates for grant applications and more available faculty positions. Despite the commendable efforts by the NIDCD in providing career development grants (e.g., R21 ECR or K grants) over the past 10 years, there were only two K99s, six Fs and six R03s that were OM-related. In addition, there was only one T32 program that included OM research. Moreover, some postdocs trained in OM research choose to pursue other career opportunities. The challenge is to determine what special efforts we can make to attract more young scientists to OM research at various stages of their career (B.S., Ph.D., postdoctoral fellow, and junior faculty). The OM community needs to continue active efforts to publicize the importance of OM, particularly within the global context, to retain trainees and attract potential trainees/young researchers who are currently working outside the OM field.
Summary: Many challenges faced by OM researchers apply to the entire biomedical field. However, challenges may be turned into opportunities (e.g., less competition) that are favorable for PIs, trainees, and early career researchers (ECRs). Reduced competition also allows for more collaborations among OM researchers and with those outside the field, enhancing opportunities for trainees/ECRs. For OM, many research areas remain untapped and can be pursued by trainees/ECRs.
Proposed strategies within the focus areas
- Stress the serious health and socioeconomic burden of OM in the developing world, and in other underserved populations, in grant applications: The community of OM grant reviewers needs to be educated about the seriousness of OM. Strong statements, supported by data, should stress the magnitude of OM as a clinical problem within the mission of the NIDCD; the mortality and especially the morbidity of OM in countries and populations with limited access to medical care; the effects of OM in vulnerable ethnic and genetic populations; and the socioeconomic effects of severe hearing loss in developing countries and underserved populations where treatments for hearing loss, including hearing aids, are cost-prohibitive.
- Increase visibility of OM research in undergraduate and graduate education: Stress the continued relevance of OM (acute, chronic, suppurative, cholesteatoma) in developed and developing countries, the polymicrobial etiology of disease, the impact of advanced genomics and new technologies, multi-omic studies, strain evolution, epidemiology, etc., in OM research and in the context of observations/advances in other fields that are “hot topics” (parallels in observations with other microorganisms in biofilm, metabolomics, genomics, pathogenesis, immunity, pharmacology, other organ systems with similar disease mechanisms, e.g., lung, virology/infectious diseases).
- Recruit and invest in talent: Seek out and provide training opportunities for trainees at all levels (research technicians, graduate students, medical students, postdoctoral fellows). Success depends upon willing staff and PIs to invest in training/mentoring; adequate support to hire new trainees; established networks in academic, industrial, and institutional settings to foster trainee interactions with the scientific community; presentation/ publication of research in local, national, and international forums; providing leadership opportunities/development of junior researchers as trainee representatives on boards, planning committees, etc.; support of succession planning; and mentors’ hands-on guidance.
- Encourage trainees and young faculty to participate in activities that may not be directly related to producing research data but may increase their chances of success in their future careers as OM researchers: Opportunities in campuses, research organizations, and societies such as ISOM include: attendance in annual/biennial meetings where other OM researchers are available to exchange research ideas and where they gain experience and exposure in presenting their OM findings; organization of OM symposia; pursuit of awards designed for trainees and junior faculty; and workshops for grant writing, science leadership, and clinical trials. When invited, ECRs should be encouraged to serve as academic editors, editorial board members of journals, and members of study sections or technical review panels.
- Support cross-discipline research (collaborative expertise): Expand OM research affinity groups within and between institutions. Collaborations facilitate cross-training of junior researchers. Collaboration with researchers working on diseases with similar mechanisms of inflammation or infection across organ systems (e.g., lung/skin diseases, hearing loss, genetic syndromes, immunodeficiencies) may also facilitate interest from groups that have additional access to resources (established human cohorts, patient databases, animal models, new technologies, analysis techniques, consortia/networks including conduct of clinical trials). Likewise, OM research may contribute to understanding of other systemic diseases. Cross-discipline research can also facilitate the development of new avenues of translational OM research.
- Advocate for OM research in any possible forum: Scientific meetings, public health forums, community outreach, publications (journals or book chapters), and press releases can publicize OM. For advocacy, it is important to generate new data on OM epidemiology by type/definition (not only within the U.S., but also globally), on pathogenesis, and on morbidities such as hearing loss and cholesteatoma. Additional support from foundations or industry could facilitate an increase in the OM workforce that is a critical need in the clinical translation of OM-related basic science findings.
- Leverage cutting-edge techniques to attract people to the field: More rapid adoption of advanced methods could help attract new students. This includes advances in conditional and site-specific mutagenesis, epigenetics, nanobiology, advanced proteomics, CRISPR-Cas9, and others that have yet to be applied to OM research.
Summary and conclusions
The NIDCD Working Group on Otitis Media in Childhood has identified major gaps in our understanding of OM that present opportunities for novel and continued research. The group has also noted important barriers to progress in the field, in clinical and basic research, and in translation of research to the clinic. Within the sections of the working group, certain topics were repeatedly raised. They include, in no particular order, the need to:
- Document the true burden of OM worldwide.
- Publicize the magnitude of OM as a health burden.
- Enable clinical trials for NTHi and Mcat vaccines.
- Increase the translation of basic research to clinical utility.
- Use cutting-edge and novel methods to advance the field of OM research.
- Better understand immune responses in the middle ear (ME).
- Increase omics and genetic studies to better understand pathogenesis and recovery.
- Study the microbiome relationships of the ME, the nasopharynx, and potentially the gut.
- Broaden collaboration with laboratories outside the field of OM.
- Establish formal research consortia of OM groups to leverage the efforts of the OM research community.
- Renew the workforce in OM research.
This report is respectfully submitted to the NIDCD with the goal of significantly advancing the institute’s portfolio of OM research.

