On this page:
- What is otosclerosis?
- How do we hear?
- What causes otosclerosis?
- What are the symptoms of otosclerosis?
- How is otosclerosis diagnosed?
- How is otosclerosis treated?
- What kinds of research on otosclerosis does the NIDCD support?
- Where can I find additional information about otosclerosis?
What is otosclerosis?
Otosclerosis is a term derived from oto, meaning “of the ear,” and sclerosis, meaning “abnormal hardening of body tissue.” The condition is caused by abnormal bone remodeling in the middle ear. Bone remodeling is a lifelong process in which bone tissue renews itself by replacing old tissue with new. In otosclerosis, abnormal remodeling disrupts the ability of sound to travel from the middle ear to the inner ear. Otosclerosis affects more than three million Americans. Many cases of otosclerosis are thought to be inherited. White, middle-aged women are most at risk.
How do we hear?
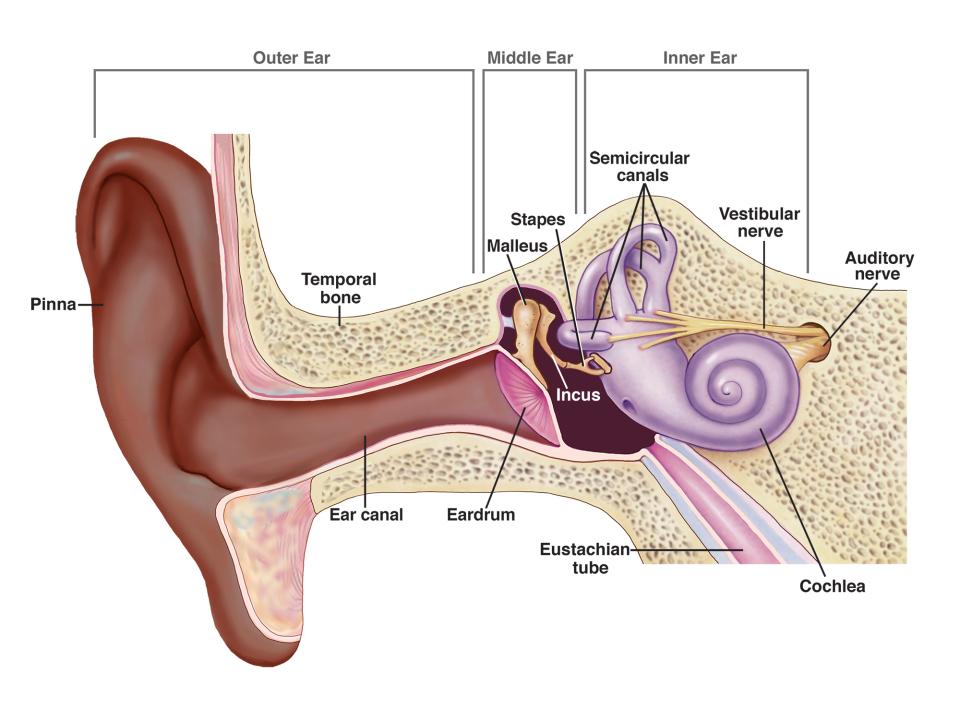
Healthy hearing relies on a series of events that change sound waves in the air into electrochemical signals within the ear. The auditory nerve then carries these signals to the brain.
First, sound waves enter the outer ear and travel through a narrow passageway called the ear canal, which leads to the eardrum.
The incoming sound waves make the eardrum vibrate, and the vibrations travel to three tiny bones in the middle ear called the malleus, incus, and stapes—the Latin names for hammer, anvil, and stirrup.
Hair cells in the inner ear
Under great magnification, hair cells can be seen as
the arrow shaped structures at the top of the photo.
The middle-ear bones amplify the sound vibrations and send them to the cochlea, a fluid-filled structure shaped like a snail, in the inner ear. The upper and lower parts of the cochlea are separated by an elastic, “basilar” membrane that serves as the base, or ground floor, upon which key hearing structures sit.
Incoming sound vibrations cause the fluid inside the cochlea to ripple, and a traveling wave forms along the basilar membrane. Hair cells that sit on top of the membrane “ride” this wave and move up and down with it.
The bristly structures of the hair cells then bump up against an overlying membrane, which causes the bristles to tilt to one side and open pore-like channels. Certain chemicals then rush in, creating an electrical signal that is carried by the auditory nerve to the brain. The end result is a recognizable sound.
Hair cells near the base of the cochlea detect higher-pitched sounds, such as a cell phone ringing. Those nearer the middle detect lower-pitched sounds, such as a large dog barking.
What causes otosclerosis?
Otosclerosis is most often caused when one of the bones in the middle ear, the stapes, becomes stuck in place. When this bone is unable to vibrate, sound is unable to travel through the ear and hearing becomes impaired (see illustration).
Why this happens is still unclear, but scientists think it could be related to a previous measles infection, stress fractures to the bony tissue surrounding the inner ear, or immune disorders. Otosclerosis also tends to run in families.
It may also have to do with the interaction among three different immune-system cells known as cytokines. Researchers believe that the proper balance of these three substances is necessary for healthy bone remodeling and that an imbalance in their levels could cause the kind of abnormal remodeling that occurs in otosclerosis.
What are the symptoms of otosclerosis?
Hearing loss, the most frequently reported symptom of otosclerosis, usually starts in one ear and then moves to the other. This loss may appear very gradually. Many people with otosclerosis first notice that they are unable to hear low-pitched sounds or can’t hear a whisper. Some people may also experience dizziness, balance problems, or tinnitus. Tinnitus is a ringing, roaring, buzzing, or hissing in the ears or head that sometimes occurs with hearing loss.
How is otosclerosis diagnosed?
Otosclerosis is diagnosed by health care providers who specialize in hearing. These include an otolaryngologist (commonly called an ENT, because they are doctors who specialize in diseases of the ears, nose, throat, and neck), an otologist (a doctor who specializes in diseases of the ears), or an audiologist (a health care professional trained to identify, measure, and treat hearing disorders). The first step in a diagnosis is to rule out other diseases or health problems that can cause the same symptoms as otosclerosis. Next steps include hearing tests that measure hearing sensitivity (audiogram) and middle-ear sound conduction (tympanogram). Sometimes, imaging tests—such as a CT scan—are also used to diagnose otosclerosis.
How is otosclerosis treated?
Currently, there is no effective drug treatment for otosclerosis, although there is hope that continued bone-remodeling research could identify potential new therapies. Mild otosclerosis can be treated with a hearing aid that amplifies sound, but surgery is often required. In a procedure known as a stapedectomy, a surgeon inserts a prosthetic device into the middle ear to bypass the abnormal bone and permit sound waves to travel to the inner ear and restore hearing.
It is important to discuss any surgical procedure with an ear specialist to clarify potential risks and limitations of the operation. For example, some hearing loss may persist after stapedectomy, and in rare cases, surgery can actually worsen hearing loss.
What kinds of research on otosclerosis does the NIDCD support?
The complicated architecture of the inner ear makes it difficult for scientists to study this part of the body. Because researchers can’t remove and analyze a sample of the inner ear from someone who has otosclerosis (or other hearing disorders), they must study ear bone samples from cadavers donated for research. These samples, called temporal bone, are in short supply. To encourage more research on otosclerosis, the NIDCD supports national temporal bone collections, such as the Otopathology Research Collaboration Network at the Massachusetts Eye and Ear Infirmary. This effort coordinates the collection and sharing of temporal bone tissue among laboratories. It also encourages scientists to combine modern biology, imaging, and computer technologies with information from patient history and pathology reports to look for new clues and solutions to ear disorders caused by bone abnormalities.
The NIDCD also funds genetic studies and bone-remodeling research to better understand the causes of otosclerosis as well as to investigate potential new treatments. NIDCD-supported researchers are currently testing—in animals—the effectiveness of an implantable device that can deliver a bone-growth inhibiting drug directly into the inner ear to correct the bone abnormalities that cause otosclerosis. If the results are promising, testing will later be done in people.
Where can I find additional information about otosclerosis?
The NIDCD maintains a directory of organizations that provide information on the normal and disordered processes of hearing, balance, taste, smell, voice, speech, and language.
Use the following keywords to help find organizations that can answer questions and provide information on otosclerosis:
For more information, contact us at:
NIDCD Information Clearinghouse
1 Communication Avenue
Bethesda, MD 20892-3456
Toll-free voice: (800) 241-1044
Toll-free TTY: (800) 241-1055
Email: nidcdinfo@nidcd.nih.gov
NIH Pub. No. 13-4234
Updated September 2013
*Note: PDF files require a viewer such as the free Adobe Reader.

