On this page:
- What is Ménière’s disease?
- What causes the symptoms of Ménière’s disease?
- Why do people get Ménière’s disease?
- How does a doctor diagnose Ménière’s disease?
- How is Ménière’s disease treated?
- What is the outlook for someone with Ménière’s disease?
- What research about Ménière’s disease is being done?
- Where can I find additional information about Ménière’ disease?
What is Ménière’s disease?
Ménière’s disease is a disorder of the inner ear that causes severe dizziness (vertigo), ringing in the ears (tinnitus), hearing loss, and a feeling of fullness or congestion in the ear. Ménière’s disease usually affects only one ear.
Attacks of dizziness may come on suddenly or after a short period of tinnitus or muffled hearing. Some people will have single attacks of dizziness separated by long periods of time. Others may experience many attacks closer together over a number of days. Some people with Ménière’s disease have vertigo so extreme that they lose their balance and fall. These episodes are called “drop attacks.”
Ménière’s disease can develop at any age, but it is more likely to happen to adults between 40 and 60 years of age. The National Institute on Deafness and Other Communication Disorders (NIDCD) estimates that approximately 615,000 individuals in the United States are currently diagnosed with Ménière’s disease and that 45,500 cases are newly diagnosed each year.
What causes the symptoms of Ménière’s disease?
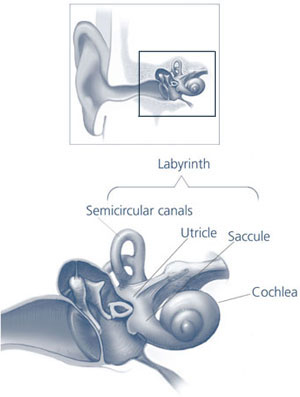
The labyrinth in relation to the ear
The labyrinth is composed of the semicircular canals, the otolithic organs (i.e., utricle and saccule), and the cochlea. Inside their walls (bony labyrinth) are thin, pliable tubes and sacs (membranous labyrinth) filled with endolymph.
Credit: NIH/NIDCD
The symptoms of Ménière’s disease are caused by the buildup of fluid in the compartments of the inner ear, called the labyrinth. The labyrinth contains the organs of balance (the semicircular canals and otolithic organs) and of hearing (the cochlea). It has two sections: the bony labyrinth and the membranous labyrinth. The membranous labyrinth is filled with a fluid called endolymph that, in the balance organs, stimulates receptors as the body moves. The receptors then send signals to the brain about the body’s position and movement. In the cochlea, fluid is compressed in response to sound vibrations, which stimulates sensory cells that send signals to the brain.
In Ménière’s disease, the endolymph buildup in the labyrinth interferes with the normal balance and hearing signals between the inner ear and the brain. This abnormality causes vertigo and other symptoms of Ménière’s disease.
Why do people get Ménière’s disease?
Many theories exist about what happens to cause Ménière’s disease, but no definite answers are available. Some researchers think that Ménière’s disease is the result of constrictions in blood vessels similar to those that cause migraine headaches. Others think Ménière’s disease could be a consequence of viral infections, allergies, or autoimmune reactions. Because Ménière’s disease appears to run in families, it could also be the result of genetic variations that cause abnormalities in the volume or regulation of endolymph fluid.
How does a doctor diagnose Ménière’s disease?
Ménière’s disease is most often diagnosed and treated by an otolaryngologist (commonly called an ear, nose, and throat doctor, or ENT). However, there is no definitive test or single symptom that a doctor can use to make the diagnosis. Diagnosis is based upon your medical history and the presence of:
- Two or more episodes of vertigo lasting at least 20 minutes each
- Tinnitus
- Temporary hearing loss
- A feeling of fullness in the ear
Some doctors will perform a hearing test to establish the extent of hearing loss caused by Ménière’s disease. To rule out other diseases, a doctor also might request magnetic resonance imaging (MRI) or computed tomography (CT) scans of the brain.
How is Ménière’s disease treated?
Ménière’s disease does not have a cure yet, but your doctor might recommend some of the treatments below to help you cope with the condition.
- Medications. The most disabling symptom of an attack of Ménière’s disease is dizziness. Prescription drugs such as meclizine, diazepam, glycopyrrolate, and lorazepam can help relieve dizziness and shorten the attack.
- Salt restriction and diuretics. Limiting dietary salt and taking diuretics (water pills) help some people control dizziness by reducing the amount of fluid the body retains, which may help lower fluid volume and pressure in the inner ear.
- Other dietary and behavioral changes. Some people claim that caffeine, chocolate, and alcohol make their symptoms worse and either avoid or limit them in their diet. Not smoking also may help lessen the symptoms.
- Cognitive therapy. Cognitive therapy is a type of talk therapy that helps people focus on how they interpret and react to life experiences. Some people find that cognitive therapy helps them cope better with the unexpected nature of attacks and reduces their anxiety about future attacks.
- Injections. Injecting the antibiotic gentamicin into the middle ear helps control vertigo but significantly raises the risk of hearing loss because gentamicin can damage the microscopic hair cells in the inner ear that help us hear. Some doctors inject a corticosteroid instead, which often helps reduce dizziness and has no risk of hearing loss.
- Pressure pulse treatment. The U.S. Food and Drug Administration (FDA) recently approved a device for Ménière’s disease that fits into the outer ear and delivers intermittent air pressure pulses to the middle ear. The air pressure pulses appear to act on endolymph fluid to prevent dizziness.
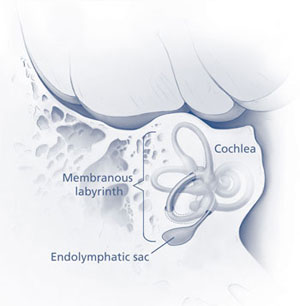
Location of endolymphatic sac
Credit: NIH/NIDCD
- Surgery. Surgery may be recommended when all other treatments have failed to relieve dizziness. Some surgical procedures are performed on the endolymphatic sac to decompress it. Another possible surgery is to cut the vestibular nerve, although this occurs less frequently.
- Alternative medicine. Although scientists have studied the use of some alternative medical therapies in Ménière’s disease treatment, there is still no evidence to show the effectiveness of such therapies as acupuncture or acupressure, tai chi, or herbal supplements such as gingko biloba, niacin, or ginger root. Be sure to tell your doctor if you are using alternative therapies, since they sometimes can impact the effectiveness or safety of conventional medicines.
What is the outlook for someone with Ménière’s disease?
Scientists estimate that six out of 10 people either get better on their own or can control their vertigo with diet, drugs, or devices. However, a small group of people with Ménière’s disease will get relief only by undergoing surgery.
What research about Ménière’s disease is being done?
Insights into the biological mechanisms in the inner ear that cause Ménière’s disease will guide scientists as they develop preventive strategies and more effective treatment. The NIDCD is supporting scientific research across the country that is:
- Determining the most effective dose of gentamicin with the least amount of risk for hearing loss.
- Developing an in-ear device that uses a programmable microfluid pump (the size of a computer chip) to precisely deliver vertigo-relieving drugs to the inner ear.
- Studying the relationship between endolymph volume and inner ear function to determine how much endolymph is “too much.” Researchers are hoping to develop methods for manipulating inner ear fluids and treatments that could lower endolymph volume and reduce or eliminate dizziness.
Where can I find additional information about Ménière’ disease?
NIDCD maintains a directory of organizations that can answer questions and provide printed or electronic information on Ménière’s. Please see the list of organizations at www.nidcd.nih.gov/directory.
Use the following keywords to help you search for organizations that can answer questions and provide printed or electronic information on Ménière’s disease:
For more information, contact us at:
NIDCD Information Clearinghouse
1 Communication Avenue
Bethesda, MD 20892-3456
Toll-free voice: (800) 241-1044
Toll-free TTY: (800) 241-1055
Email: nidcdinfo@nidcd.nih.gov
NIH Publication No. 10–3404
July 2010
For more information, contact the NIDCD Information Clearinghouse.
*Note: PDF files require a viewer such as the free Adobe Reader.

